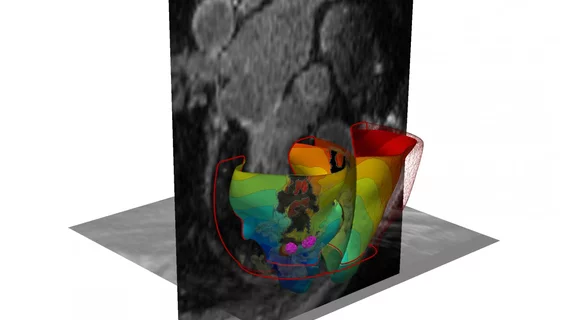
3D heart model uses MRI to pinpoint source of arrhythmia
Cardiac specialists may be able to better identify scarred heart tissue and perform cardiac ablation in arrhythmia patients with a newly developed 3D imaging system based on cardiac MRI, according to research published Sept. 3 in Nature Biomedical Engineering.
The 3D imaging technique developed by Johns Hopkins University researchers could standardize treatment and decrease the variability in outcomes for patients with ventricular tachycardia to avoid long-term risk of irregular heartbeats.
"Cardiac ablation, or the destruction of tissue to stop errant electrical impulses, has been somewhat successful but hampered by a lot of guesswork and variability in the way that physicians figure out which locations to zap with a catheter," co-author Natalia Trayanova, PhD, professor of biomedical engineering at Johns Hopkins, said in a prepared statement. "Our new study results suggest we can remove a lot of the guesswork, standardize treatment and decrease the variability in outcomes so that patients remain free of arrhythmia in the long term.”
To more accurately locate arrhythmias and improve cardiac ablation outcomes, the researchers developed 3D personalized computational models based on MRI images of the hearts of 21 patients, according to the researchers. These patients had undergone successful cardiac ablation procedures for infarct-related ventricular tachycardia between 2006 and 2017.
Each heart tissue cell in the 3D model generated electrical signals aided by mathematical equations representing how heart cells physically behave. The researchers were then able to stimulate the patients' virtual heart with small electrical signals in different locations, allowing the computer program to determine whether the heart developed an arrhythmia and where in the heart’s tissue it was caused.
Specifically, the researchers used the 3D simulation to guide cardiac ablation treatments in five patients with scarred cardiac tissue from previous procedures.
Study results included the following:
- Two patients who received the simulation-guided ablation procedure have remained free of tachycardia throughout follow-up periods of 23 and 21 months.
- One patient who had the simulation procedure remained free of tachycardia after two months of follow up.
- In two patients, the virtual heart approach predicted that tachycardia would not be inducible—this was confirmed during the clinical procedure, so cardiac ablation was not performed.
The researchers believe their findings could decrease the time of cardiac mapping, reduce patient complications and the need for supplemental procedures through its ability to make the infarcted heart incapable of producing new arrythmias, according to the release.