3D imaging technique enables customized care for mitral valve disease patients
A team of researchers from the University of Texas (UT) at Austin have developed a noninvasive 3D imaging technique that can provide surgeons customized models of the hearts of mitral valve (MV) disease patients for presurgical planning purposes, according to research published in the January issue of Annals of Biomedical Engineering.
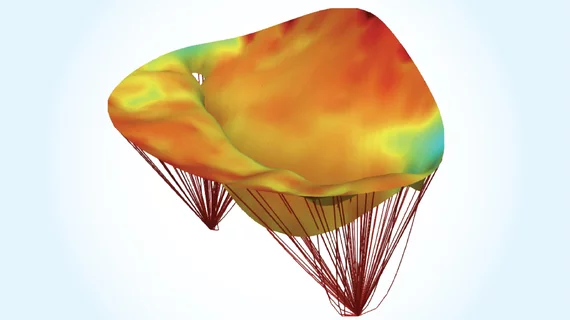
The technology is a computational modeling technique for imaging MV leaflets, which are flaps located on the base of the mitral valve which opens and closes to regulate and maintain healthy blood flow throughout the heart. The method is accurate enough to use on a case by case basis, according to the researchers.
Five million Americans are diagnosed with MV disease every year and it is one of the most common heart valve-related conditions. Heart valves are already difficult to image, but if the condition is left untreated it can lead to heart failure and/or stroke.
“Heart valves are very difficult to study. They are complex structures that move incredibly fast and are located inside the heart, making them extremely difficult to image,” lead author Michael Sacks, a professor of biomedical engineering at UT Austin, said in a prepared statement. “Our new computational model provides surgeons with a tool for the prediction of postsurgical outcomes from clinically obtained presurgical data alone.”
Using computational and 3D imaging technologies, the researchers were able to noninvasively acquire the in vivo geometry of MV leaflets in patients using real-time, 3D echocardiograms. The group's computational model was developed in collaboration with researchers from Penn Medicine in Philadelphia and Georgia Tech in Atlanta.
“To model the MV leaflets, we then integrated into the MV models the structure and mechanical properties of the internal constituents, such as the collagen fibers which make up most of the valve, to develop attribute-rich complete MV models,” Sacks said.
With their new predictive technique, the researchers hope heart surgeons will be able to customize MV leaflet repair more accurately and efficiently for each patient before undergoing surgery.
The study was funded by the National Institutes of Health.