Q&A: What updated reimbursement policies could mean for CT lung screening rates in the United States
Recent reimbursement rule changes for low-dose computed tomography (CT) lung screen scans are expected to help open up screening for more patients, according to the American College of Radiology (ACR).
The ACR recently released a detailed summary of the Centers for Medicare and Medicaid Services (CMS) National Coverage Determination related to screening for lung cancer with low-dose CT.
 To find out more details on the changes and expansion of the program, Health Imaging interviewed Alicia Blakey, the ACR's principal economic policy analyst.
To find out more details on the changes and expansion of the program, Health Imaging interviewed Alicia Blakey, the ACR's principal economic policy analyst.
Why are the CMS lung screening reimbursement changes important?
Alicia Blakey: We are really trying to increase screening uptake for lung cancer screening. Prior to these changes in the guidelines and the coverage updates, there was less than a 15% uptake rate for lung cancer screening in general. So we are definitely interested in raising awareness about the availability of the low-dose CT scans.
Can you explain more about the LDCT lung screening program and how the changes may help expand the number of patients who can be screened?
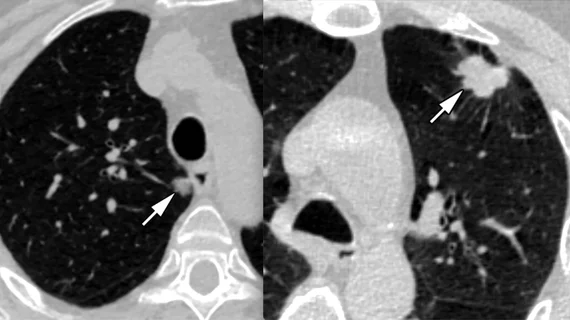
Alicia Blakey: The goal of screening is to detect disease at its earliest and most treatable stage of lung cancer, particularly in individuals who have a high risk of developing lung cancer, but do not have signs or symptoms. Lung cancer is the leading cause of cancer-related deaths in the United States, and worldwide about 85% of lung cancer deaths occur in current or former cigarette smokers. This type of cancer is most commonly non-small cell lung cancer.
The ACR was interested when the United States Preventive Service Task Force (USPSTF) issued its final recommendations in March of 2021. We were excited with the changes, because they lowered the screening age and smoking pack per-year history. These changes will expand lung cancer screening to underserved populations, such as African American women and people who do not have a long history of smoking.
The ACR also was elated when we knew that this final recommendation would expand access to lung cancer screening for the commercial payers and also Medicaid expansion states. So as an action item and an urgent request of our membership, we reached out to Medicare to make sure that they update their national coverage determination to line up with the USPSTF current recommendation for lung cancer screening.
How has the patient population changed for LDCT lung screening?
Alicia Blakey: The screening population is the most important eligibility criteria within the changes. It is now recommended that patients younger than age 55 get screened by Medicare. We've gotten several questions from membership on how many patients fall within that category. When we think of Medicare, we think of age 65 and older, and there is actually a growing millions of Americans who could benefit from this screening update, due to disability status, as well as end-stage renal disease. So there is a need for Medicare to update its coverage.
Has the shared decision-making criteria for CT lung screening changed to now include nurse practitioners and nurse navigators?
Alicia Blakey: The other notable change is that in order to do low-dose CT scans, there was a shared decision making requirement, that each visit includes counseling on smoking sensation. The old policy stated you had to be a provider or a non-physician practitioner to offer the shared decision making visit. This has now been expanded to include other auxiliary personnel incidental to a physician’s professional service.
Many of the centralized lung cancer screening programs have a have nurse navigator who schedules the patient and makes sure they schedule appointments for follow up care. This is an annual test that does require you to come back each year. So those facilities that have a nurse coordinator or navigator role are now able to order low-dose CT scans. This is another benefit of expanding the eligibility criteria to make sure that we get more patients into the office to be scanned.
Do the new Medicare rules allow for outpatient imaging centers to perform low-dose CT lung screening?
Alicia Blakey: One other notable change that the ACR was excited about is that since 2015, low-dose CT scans that were performed in an independent diagnostic testing facility (IDTF) received denied claims for all scans. In the coverage update, CMS has removed imaging facility criteria that would have prevented IDTFs from performing low dose CT scans.
IDTFs should have been able to bill Medicare for low-dose CT scan since 2015, but there were some errors and administrative barriers that have now been removed. We hope these facilities will help with screening uptake as we try to reverse course back to pre-pandemic levels. There are a lot of patients that need to be scanned.
The American Cancer Society said in its latest stats for 2021, there will be 131,000 deaths due to lung cancer. So we have a big job ahead of us to improve access to this scan, and that includes allowing all facilities to perform this life saving preventive test.
CMS dropped the requirement for registry participation. How will this impact LDCT lung screening?
Alicia Blakey: In the old rules, CMS required radiology imaging facilities to submit data to a CMS approved registry. That criteria has been removed by CMS. Their rational was that they wanted to reduce barriers to screening, and they felt low-dose CT scans had good data that was submitted on its utilization and purpose of screening eligible patients. They felt the screening service was no longer new, so registry data should not longer be required.
The ACR lung cancer screening registry is a quality improvement tool. So we are recommending people continue to submit their data so they can get meaningful measures such as cancer detection rates and making sure that they're screening the eligible population.
Do you have any idea what how many of these screening exams are performed each year and how many cancers are actually caught using this process?
Alicia Blakey: The ACR operated the only CMS-approved lung cancer registry, which was started in February 2015. So there has been significant data collected on the number of screening exams taking place, and whether or not eligibility criteria is being met. We publish this information on our website as well as information for our screening centers that are designated screening centers of excellence.
In 2021, we had a 3,593 facilities participating. That includes hospitals and medical groups performing the low-dose CT scans participating in the ACR Lung Cancer Screening Registry. There were 866,954 lung screening exams performed just in 2021.
A lot of hospitals used LDCT lung screening to schedule more patients on that underutilized scanners, is this still true?
Alicia Blakey: You are actually correct. The hospitals are currently using their existing CT equipment to perform these exams. So there is no extra costs or burden of purchasing of new equipment specific to lung cancer screening.
Overall, is the ACR hoping changes in Medicare reimbursements will help boost the expansion of the LDCT lung screening program?
Alicia Blakey: Yes, absolutely. We see that CMS analysis group updating their coverage guidance to model the U.S. Preventive Task Force recommendations should essentially allow more patients to be scanned at no cost. With CMS updating its eligibility criteria, we are certain that it will increase the ability of more people to obtain access to screening. The coverage decision memo that was released on Feb. 10, 2022, is the effective date, so Medicare will reimburse providers for performing the low-dose CT scan if all of the National Coverage Determination (NCD) criteria is met.
Can you tell me about the Medicare reimbursement rates for LDCT lung screening between 2015 to today?
Alicia Blakey: In November each year, CMS releases its Medicare Physician Fee Schedule as well as its hospital outpatient perspective system proposed and final rules. All of these changes were effective Jan. 1, 2022. We've had some very good news to come out of our Hospital Outpatient Prospective Payment System (HOPPS) regarding the low-dose CT scan CPT code 71271.
In previous years, our previous code G0297 and 71271 had been placed in a lowest imaging without contrast Ambulatory Payment Classifications (APC) with a payment rate around $83. The ACR over several years has raised concerns about the inadequate payments of CT lung cancer based on flawed hospital data. So we were elated and excited about the increased reimbursement that came as a result of the 2022 final rule.
The ACR is very pleased that CMS has reassigned CPT code 71271 to the second tier imaging without contrast APC. And this second tier has a higher reimbursement rate of $111.19. We are excited for some increased reimbursement.
Our facilities are doing a lot of work to make sure that patients are eligible and that they are using things like Lung-RADS, which is a quality assurance tool designed to standardize lung cancer screening CT reporting and management recommendations. It is more than just a CT scan, it is an involved and sophisticated program.
I would say for the Medicare Physician Fee Schedule, the rates are comparable. There was not a significant increase as we saw with the hospital outpatient, but for the Medicare Physician Fee Schedule, which would capture anyone who bills Medicare Part B services in a physician setting or a imaging facility, the global rate for that is now $147. It was $150 in 2021, so that is a slight decrease. We do always recommend that CMS align their reimbursement rate with our CT chest code 71250.
Overall, we are fine with these changes in the Medicare reimbursement rates.
Does ACR offer resources for patients who want a low-dose CT lung screening?
Alicia Blakey: We want them asking about lung cancer screening and we have a wealth of resources available for patients and referring providers. We have a lung cancer screening locator tool, which is available on our website, and we have a webpage dedicated to patient information about the low dose at www.radiologyinfo.org/en/info/screening-lung.
Read more details on the ACR's review of the CMS lung screening changes
Related LDCT Lung Screening Content:
CMS expanding coverage for CT lung cancer screening, drawing imaging advocate praise
For first time, large population-based study proves CT screening reduces lung cancer deaths
Stand-alone AI for lung cancer screenings could reduce radiologist workloads by 86%, study suggests
Are LDCT lung screening programs overdiagnosing cancer?
ACR outlines changes in Medicare lung cancer screening coverage
Rural lung cancer screening program boosts engagement, with nearly 90% of LDCT orders completed
New research sheds light on imbalance in cancer imaging studies
Presidential call to action on cancer screening draws praise from radiology community
Rural veterans less likely to get LDCT lung cancer screenings, prompting doctors to call for change
Radiologists and thoracic surgeons voice concerns over CMS proposal to expand lung cancer screening
ACR seeking changes to CMS proposal that would expand eligibility for CT lung cancer screening