Common MRI findings in 'foot drop' cases
A new paper in the European Journal of Radiology offers an updated overview of common MRI findings in patients who develop foot drop following total hip arthroplasty (THA).
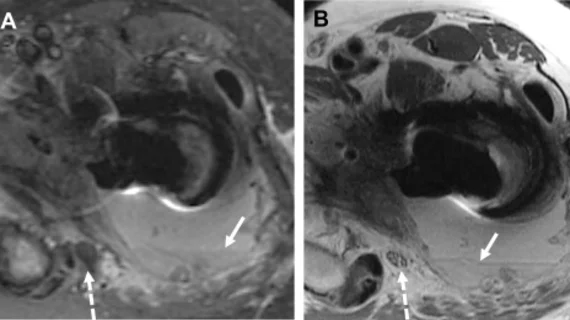
The most common surgical method of THA involves a posterior approach. While the operation is safe overall, this approach can sometimes leave patients with sciatic nerve injuries in the immediate weeks following surgery. These rare injuries can result in “foot drop” for some patients, making it difficult for them to maneuver the front of their foot.
“While new onset foot drop can be multifactorial, in patients with recent hip surgery, pathology is most commonly localized to the surgical site,” corresponding author of the new paper Darryl B. Sneag, with the Department of Radiology and Imaging at the Hospital for Special Surgery in New York, and co-authors explained.
Sneag and colleagues noted that advances in MRI technology have improved clinicians’ ability to visualize the peripheral nerves within the vicinity of newly placed metallic hardware in THA patients. Proper characterization of nerve injury patterns could better inform management, the authors suggested.
To better understand patterns associated with foot drop, the group retrospectively analyzed 51 cases of patients who had undergone MRI for the condition within four weeks of posterior-approach THA surgery over a 20-year period.
They observed the following on imaging:
Compression of the sciatic nerve by edema or a fluid collection, without intrinsic nerve abnormality in 19 patients
Perineural tethering or scar tissue encasement of the nerve, with fluid-sensitive sequences revealing the sciatic nerve to be enlarged in half of the patients
Sciatic nerve compression secondary to quadratus femoris retraction in six patients
Six patients’ foot drop completely resolved at a mean follow-up of 37.3 months, but those patients’ postoperative MRI scans did not display sciatic nerve injuries. All other patients continued to experience weakness in the 34 months following their surgery.
The experts noted that these cases occurred over a 20-year period, and many were conducted using a 1.5 Tesla MRI. They suggested that 3T imaging is more suitable for nerve visualization and that standard high resolution 2-D sequences are preferable over multispectral techniques. Regardless of protocol, the authors advised that radiologists should supervise MRI examinations in foot drop cases so that sequences can be adjusted as needed.
To learn more, click here.