Fine Line: Gender Disparities in Cardiac Disease Management
Coronary artery disease is the leading cause of death in women, according to the Centers for Disease Control and Prevention. It takes the life of more than 300,000 women annually, nearly 10 times that of breast cancer. Yet, imaging—often the bedrock for first diagnosing and then treating cardiac disease—remains challenging and inconsistent in women. Understanding gender differences in the physiology, symptoms and risk factors can help narrow the gender gap and improve the utility of cardiac imaging.
Previously stereotyped as a "man's disease," coronary artery disease represents a serious risk for women. It is more prevalent in men—8.3 percent of adult men are currently living with the condition compared with 6.1 percent of adult women, according to the American Heart Association's 2011 Statistical Update—but women are more likely to die from a first myocardial infarction and also experience more long-term disability living with CAD.
In addition, certain populations of women are at higher risk. Obese women, and those with diabetes, have increased incidence rates, and the risk doubles for post-menopausal women.
Although physicians have become more aware of the seriousness of heart disease in women, a gender disparity in treatment persists. Of patients with angina, a woman's odds of being referred for coronary angiography were 59 percent that of a man's, and women also are less likely to undergo an exercise ECG, according to a study published in January 2006 in Circulation.
Differences in testing and treatment may be due to gaps in knowledge about symptom presentation and risk factors, with some physicians not making the adjustments to provide gender-specific care.
One potential problem, according to Leslee J. Shaw, PhD, co-director of the Clinical Cardiovascular Research Institute at the Emory University School of Medicine in Atlanta, is that the profile of female patients is changing.
"We don't have a female-specific description of anginal symptoms," Shaw says. "Many of the women who present with anginal symptoms are classified as more atypical because they could be not exertion-related … and don't present with that typical 'Hollywood heart attack', such as shoveling snow or mowing the lawn."
Women may present with shortness of breath, which Shaw believes is underdiagnosed, and their angina may be stress-triggered as opposed to exertion-related. Other atypical symptoms include indigestion, nausea and discomfort in the elbow or jaw.
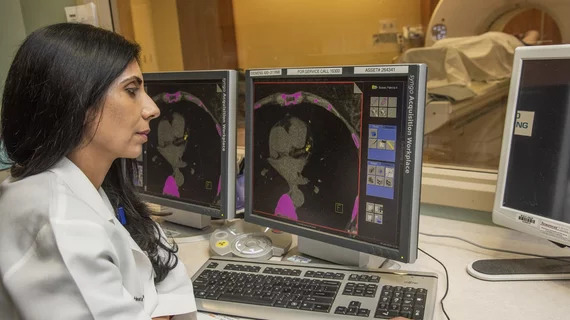
Cardiac imaging for women underused and unnecessary?
Over the last few decades, the use of myocardial perfusion imaging (MPI) to diagnose coronary artery disease has increased threefold, with a rate of utilization among Medicare beneficiaries of 8,467 per 100,000.
After examining these data, researchers identified another disparity: a higher percentage of women receive tests who do not meet appropriate use criteria.
Aarti Gupta, MD, a cardiology fellow at Miriam Hospital and Rhode Island Hospital, both in Providence, R.I., and colleagues conducted a study, published in the Journal of Nuclear Cardiology in August, of 314 consecutive MPIs and found women accounted for 68 percent of the inappropriate tests and 82 percent of the uncertain tests.
This presents a fine line for physicians. Women are under-tested, but a higher percentage of unnecessary tests occur in women referred for MPI.
"It's not always clear," says Gupta. "Our study shows that we are testing more women with nuclear stress tests than perhaps need the test, but, at the same time, we do not want to miss women with heart attacks as women can present with atypical symptoms."
Another finding of Gupta et al was that cardiologists were more likely than primary care physicians to order tests classified as appropriate at a rate of 86 percent compared to 71 percent, respectively. Gupta says the American College of Cardiology's guidelines for appropriate use of nuclear stress testing would help. The hitch? Primary care physicians aren't referencing the guidelines.
"This guideline document has been circulating in the cardiology community since 2005, but it has not become very prevalent in the primary care community," says Gupta. "We need to do more to educate primary care physicians to help them select patients for testing more appropriately."
Cardiac anatomy, imaging and economics
William E. Boden, MD, of the University at Buffalo School of Medicine and Public Health in New York, offers a theory for the number of negative nuclear imaging tests in women. Boden explains that women have a different syndrome that causes ischemia. Rather than a narrowing or blockage of the epicardial coronary artery, women are likely to have microvascular angina involving small microvessels that are not delineated with a coronary angiogram. Evidence of ischemia may be on the ECG, but a report from the cath lab shows normal coronaries.
"So I'm not really sure it's a false positive," says Boden. "It may be a true positive, but it's not due to narrowed epicardial coronaries. It may be due to microvascular angina."
Recent studies have looked into the theory of gender-specific heart attack. Researchers at the Cardiac & Vascular Institute at NYU Langone Medical Center in New York City used intravascular ultrasound and cardiac MRI to discover that 38 percent of heart attacks in women with normal angiograms were triggered by plaque disruption that could not be seen on an angiogram.
To avoid false positives that result from these forms of ischemic heart disease, some physicians may be inclined to skip over the ECG, which guidelines suggest as an initial test, and proceed straight to MPI. To determine the benefits of different approaches, Boden, Shaw and others conducted the What Is the Optimal Method for Ischemia Evaluation in Women (WOMEN) Trial that examined the benefits of MPI over traditional ECG exercise testing. Prior to the trial, most researchers believed MPI combined with a treadmill test would be better than treadmill alone, Boden explains.
They were wrong. "It turns out that treadmill exercise testing was as good as perfusion imaging and, obviously, it was far less costly. Perfusion imaging was not superior to standard treadmill exercise in terms of predicting events at follow-up," says Boden.
A total of 824 women were randomized to either a standard treadmill test or an exercise MPI. ECG results on the treadmill test were normal for 64 percent of women, indeterminate for 16 percent and abnormal for 20 percent. MPI results were normal in 91 percent, mildly abnormal in 3 percent and moderate to severely abnormal in 6 percent. At two years post-test, there was no difference in major adverse cardiac events.
In addition to providing a diagnostic advantage, treadmill testing is more economical. In the WOMEN trial, patients randomized to the standard treadmill test had diagnostic costs 48 percent lower than the exercise MPI group. If more women at low and intermediate risk of coronary artery disease were given treadmill tests as an initial diagnostic test, it could result in considerable cost savings, as two million to three million women undergo exercise MPI annually.
The findings, according to Boden, should reinforce current guidelines and could save money if followed, but hospitals may feel pressured to order tests to justify the purchase of imaging equipment. Plus, as long as Medicare and other payors keep paying, there's no incentive to order fewer tests.
"We should start applying evidence-based medicine," says Boden. "We all worship at the altar of evidence-based medicine, but we practice it selectively."
However, there is a gray area as evidence-based medicine has not yet identified definitive gender-based protocols. That is, more research is needed to determine the best course of action for female patients and to help physicians walk the fine line between under-aggressive treatment and unnecessary imaging studies.