New DL model detects effects of long COVID using only x-rays
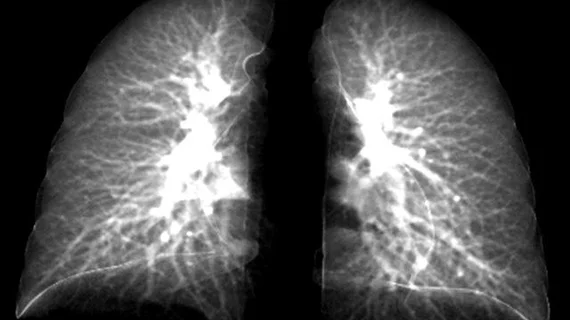
Researchers at the University of Iowa have developed a new deep learning model that can detect lung abnormalities on 2D chest radiographs as if they were obtained using more detailed 3D computed tomography technology.
Experts involved in the model’s development suggested that it could be beneficial in areas where CT scans are not readily available, especially in the cases of patients who suffer from long COVID.
“The new element to the model is taking information from 3D CT scans showing lung volume and transferring that information to a model that will show these same characteristics in 2D images,” Ching-Long Lin, chair of the Department of Mechanical Engineering in the College of Engineering at Iowa, said in a release. “Clinicians would be able to use chest X-rays to detect these outcomes. That’s the bigger perspective.”
The model uses composite 2D images constructed from 3D images to detect alterations in lung function of COVID patients.
To create the model, the researchers used the CT imaging from 140 patients who had been infected with COVID and treated at UI Hospitals & Clinics for respiratory issues. The imaging contained acquisitions completed during both inhalation and exhalation and was compared to exams from a group 105 of patients who had never contracted COVID. Using this imaging, the model was trained to differentiate between healthy patients and those with COVID, in addition to being able to identify post-COVID-19 subtypes.
The model achieved an accuracy of 90% in differentiating between the COVID group and the healthy controls. In addition to this, the model identified two distinct clusters of characteristics among the patients with long COVID—one group with increased air-trapping caused by small airways disease and diffusing capacity for carbon monoxide, and another group with decreased lung volume and increased ground glass opacity.
When applied to chest imaging, the model can capture features of two post-COVID subtypes characterized by air-trapping due to small airways disease and airway-associated interstitial fibrotic-like patterns.
Lin noted that while CT scans are not always accessible, X-rays typically are. In instances where accessibility is a challenge, Lin and colleagues believe that their model could help close the care gap.
“Our model can be further improved, and I believe there is potential for it to be used at all clinics without having to buy expensive imaging equipment, such as CT scanners.”
The detailed research can be viewed in Frontiers in Physiology.
The release about the new work can be viewed here.