MRI analysis offers new insight into vaccine-related lymphadenopathy in the general population
A new paper published in Radiology offers updated insight into the presentations of COVID vaccine-related lymphadenopathy—this time as visualized on chest MRI exams.
To date, research pertaining to reactive lymphadenopathy has focused mostly on patients with cancer who are routinely staged and monitored via PET/CT or in women undergoing breast cancer screening and/or imaging with mammography and ultrasound. While these studies have helped mold current recommendations regarding the the timing of imaging after COVID vaccination in these patients, there remains a lack of data regarding a more general population, authors of the study suggested.
“Recommendations in the early days of 2021 are provisional, and more appropriate management strategies for vaccination-related lymphadenopathy are needed in both the general population and high-risk oncology patients,” corresponding author of the paper Takeharu Yoshikawa, of the Department of Computational Diagnostic Radiology and Preventive Medicine at the University of Tokyo Hospital, and colleagues wrote [1].
This study sought to add to the conversation with data that include both men and women—300 males and 133 females, to be exact—of varying ages. Pre- and post-vaccination chest MRIs were obtained for each patient from June to October 2021. Various metrics were compared between the two scans, including imaging features and other patient health data (time of vaccination, age, etc.).
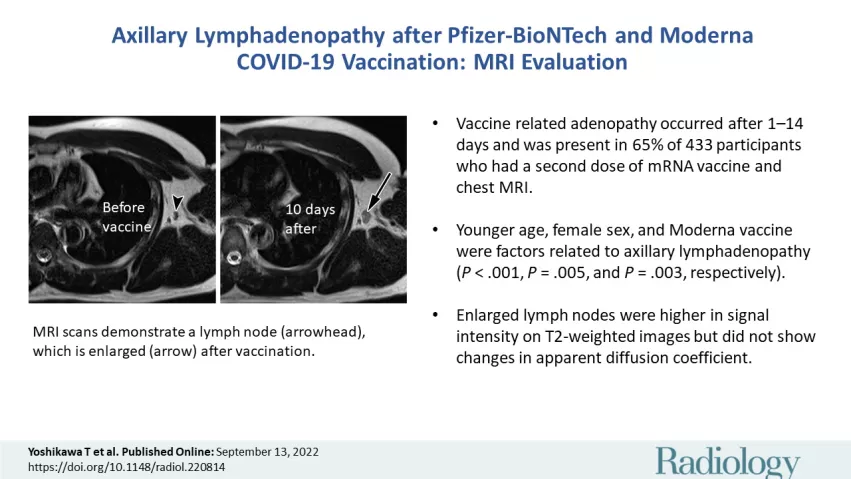
Researchers found that 65% of patients displayed axillary lymphadenopathy between 1 to 14 days after receiving the second dose of their vaccination; these findings persisted for at least 43 to 56 days in 18%. Several factors were revealed to be predisposing factors for the reactive adenopathy in these patients, including being female, younger in age and having received a Moderna, rather than Pfizer, vaccine.
Just 2% of patients had five or more enlarged nodes, with those measuring 10 mm or higher seen in 1%. The experts shared that enlarged nodes demonstrated higher signal intensity on T2WI, but ADC remained within normal range.
Based on their findings, the experts suggested that nonurgent chest imaging should be delayed in recently inoculated patients, especially in the first 1 to 14 days, so as to avoid false positives that could lead to additional imaging and procedures.
To learn more about the study, click here.