Life-threatening barotrauma common in intubated COVID patients, trackable by chest X-rays
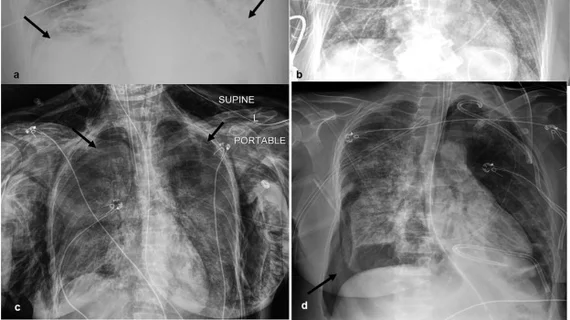
Mechanically ventilated COVID patients face an increased risk of barotrauma, which can lead to additional complications such as pneumomediastinum, subcutaneous emphysema, pneumothorax and even death.
A recent paper published in Clinical Imaging took a closer look at the incidence of barotrauma, how it presents on imaging and the increased risks related to mechanical ventilation poses to COVID patients. Researchers found that intubated patients with radiographically present barotrauma had increased odds of death compared to patients without the procedural complication.
“The literature describing the relationship between barotrauma and mortality is complex with many studies reporting an increased risk of mortality in the mechanically ventilated population. However, in these studies, barotrauma is likely not the direct cause of death in most patients but rather a marker for illness severity,” corresponding author Sharon Steinberger, with the Division of Pulmonary, Critical Care, and Sleep Medicine at the Icahn School of Medicine at Mount Sinai, and colleagues explained.
Researchers included 363 intubated COVID patients in their analysis, 43 (12%) of whom developed barotrauma radiographically. In the barotrauma group, 95% developed pneumomediastinum and subcutaneous emphysema a median of 2 days post-intubation. Pneumothorax was spotted on imaging in 40% of barotrauma patients, compared to just 3% in the group without barotrauma. These findings typically presented within 7 days of ventilation. Of note, the researchers shared that they did not uncover statistically significant associations between barotrauma and ventilatory pressures and volumes.
Barotrauma patients were found to have a 7% increase in mortality compared to their peers and 60% died before the resolution of the complication. In the patients who survived, barotrauma resolved in an average of 5 days.
“The spontaneous resolution supports the theory that barotrauma is not the direct cause of death in most patients but can lead to complications such as pneumothoraces and is likely a marker for illness severity,” the experts suggested.
They continued by indicating that radiologists involved in the care of these patients should be especially vigilant in identifying the signs of complications in these patients.
More on COVID complications:
Detailed MRI reveals pulmonary vascular abnormalities in COVID long-haulers
NIH grants $3.5 million toward researching COVID's neurological impact
New imaging technique detects post-COVID lung abnormalities
Intrathoracic complications in COVID patients: Incidence, associations and outcomes
Reference:
Sharon Steinberger, Mark Finkelstein, Andrew Pagano, Sayan Manna, Danielle Toussie, Michael Chung, Adam Bernheim, Jose Concepcion, Sean Gupta, Corey Eber, Sakshi Dua, Adam H. Jacobi. Barotrauma in COVID 19: Incidence, pathophysiology, and effect on prognosis. Clinical Imaging, 2022.