Experts call for reporting guidelines for breast arterial calcifications identified on mammo
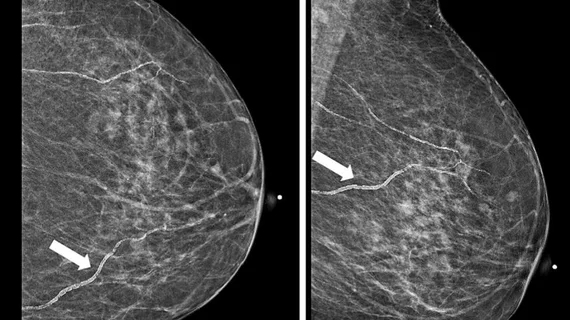
Many referring providers are unaware of the association between breast arterial calcifications (BAC) and increased cardiovascular risk, though most agree that information regarding the finding should be included in mammography reports.
BACs and cardiovascular risk have been a growing topic of conversation in recent years, as numerous studies have indicated there could be a relationship between the two. Despite this, there are no standard reporting requirements related to BACs. This could be due, at least in part, to a lack of awareness, according to new survey responses published in the Canadian Association of Radiologists Journal. Those responses revealed as few as 17% of referring providers are familiar with the relationship between BACs and cardiovascular risk.
The knowledge gap could be contributing to missed opportunities to improve patient care, experts involved in the analysis suggested.
“Reporting of BAC on mammography may prove a useful opportunistic screening tool to identify those at increased cardiovascular risk, given that just over half of eligible Canadians aged 50 to 69 undergo regular screening mammography,” corresponding author Charlotte J. Yong-Hing, with the department of radiology at the University of British Columbia, and colleagues noted. “This presents a unique opportunity for radiologists to provide additional insight into an individual’s cardiovascular risk, which may aid in prevention of adverse cardiovascular events by facilitating lifestyle modification, further investigation, or initiation or escalation of care.”
Despite less than 20% of the 72 physician respondents being familiar with BAC-associated risk, more than half indicated that the finding should be included in mammography reports. Fifty-six percent said that the finding would likely prompt them to initiate further investigation and 63% said they would inform patients of the presence of BACs.
In terms of reporting standards, 69% suggested that a BAC grading system would be beneficial and 71% agreed that national reporting guidelines are needed.
Informing patients of BACs found on their mammogram could add additional burden, however, the authors noted. This could include increasing both patient stress and cardiology referrals, some of which may be unnecessary.
“Some physicians felt that they would still feel obligated to always notify patients with BAC (e.g., if observed on an otherwise negative or benign mammogram who were already on primary or secondary preventative therapy for cardiovascular risk factors), even if they were not making meaningful changes to the care plan,” the group wrote, adding that these factors further emphasize the need for BAC reporting and clinical management guidelines.
Learn more about the survey results here.