Commercially available AI tool detects 76% of PE that rads initially missed on CT
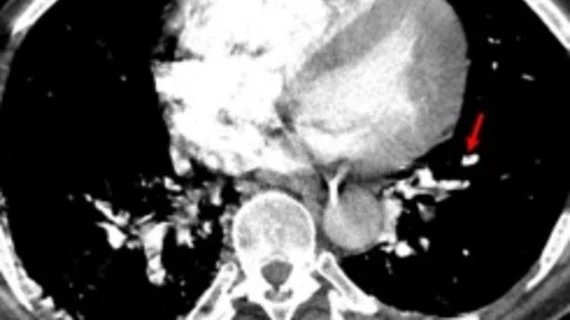
An artificial intelligence-based algorithm can significantly reduce miss rates for pulmonary embolism (PE) on CT imaging, according to new work published in Clinical Imaging.
The retrospective study, which included more than 1,200 CT pulmonary angiography (CTPA) exams, revealed the algorithm’s performance to be consistent across dozens of scanner models and vendors. Its use resulted in identifying 76% of PE that the reporting radiologists initially missed.
Accuracy and consistency in spotting PE varies widely among radiologists, the authors noted. As such, PE diagnosis has been a target of multiple AI vendors.
For this study, experts analyzed a CE-marked and FDA cleared DL-based algorithm (CINA-PE) at a per-case level (PE detection and prioritization) and at a per-finding level (secondary captures for PE location)—something that not all AI tools within the realm of PE detection have been put through, the group suggested.
The tool was put to the test on CTPA exams collected across 230 U.S. cities and acquired on 57 different scanner models from six different vendors. The exams were first interpreted by three board certified radiologists to establish ground truth, and then by the AI tool. The new interpretations from both the radiologists and the AI tool were compared to each other and to the initial exam reports.
A total of 1,204 CTPAs were included in the analysis. The tool achieved a per-case sensitivity and specificity of 93.9 % and 94.8 %, and a positive predictive value of 89.5%.
There were 196 total positive cases, 29 of which were not mentioned in the initial clinical report. Of those, AI detected 22, or 76%, of PE, reducing the miss rate from 15.6 % to 3.8 %—a finding that could have life-altering consequences for some patients, the group suggested.
“In addition to the potential impact on the PE clinical workflow, this type of CAD solutions may decrease the number of missed PE by on-call radiologists, especially during night shifts or large workload periods,” Peter D. Chang, MD, with the Department of Radiological Sciences at the University of California Irvine, and colleagues noted. “DL-based tools embedded in radiology clinical workflow can be leveraged to rapidly detect challenging cases and prevent potential misdiagnosis. This accurate analysis can result in timely interventions and better patient management.”
Though the software has great clinical utility, the group acknowledged that all AI tools must be “continuously and rigorously evaluated.”