New protocol addresses contrast allergies in patients with suspected stroke
Experts at Mayo Clinic have developed an imaging protocol for cases when patients with suspected stroke have a history of severe adverse reactions to contrast media.
Contrast allergies are not incredibly common and most are mild, but there are rare occasions when the use of iodinated contrast can be life-threatening due to previous serious reactions. In patients with suspected stroke, this presents a significant dilemma, as contrast-enhanced imaging offers providers greater visualization of potential abnormalities.
“Despite the well-established safety of IV contrast, hesitancy to administer contrast when indicated in patients with known or suspected allergies leads to significant delays in patient care,” Gabriel M Virador, MD, with the Department of Radiology at Mayo Clinic in Jacksonville, and colleagues noted. “While there are varying recommendations, there is no consensus for the optimal imaging of stroke patients with prior anaphylactic reactions to iodinated contrast.”
Most protocols related to contrast allergies involve administering pre-scan medications—typically a combination of corticosteroids and antihistamines—several hours prior to CT imaging. However, this isn’t feasible in stroke patients, as the sooner their imaging is completed, the sooner clinicians can initiate appropriate treatments.
In the absence of recommendations specific to stroke patients with contrast allergies, the team sought to develop a standardized protocol at their institution in hopes it would expedite care for those vulnerable to severe contrast reactions. To do this, the team consulted all relevant staff, including radiologists, emergency providers, neurologists, nurses and technologists.
Here’s what the team came up with:
When patients with suspected stroke present to the ED, the emergency provider in charge of their care immediately contacts the radiologist to seek approval for contrast use.
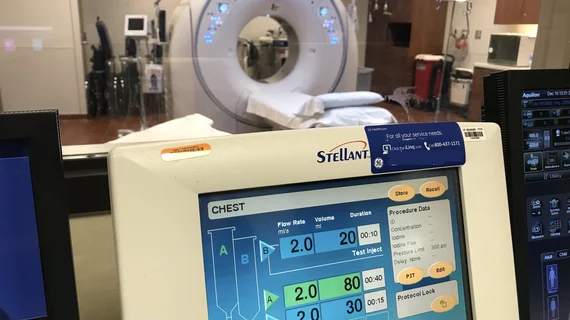
The radiologist determines whether contrast-enhanced CT is warranted or if MRI would be more appropriate. If contrast-enhanced CT is deemed appropriate, providers determine whether the use of a different class of contrast is an option. For example, if the inciting agent was an iso-osmolar contrast, such as iodixanol, using a low-osmolar contrast agent, such as iohexol, could be a safer alternative.
While the radiology department is approving imaging plans, support staff works to obtain consent to both administer contrast and initiate pre-scan medication.
Pre-medication—typically 200 mg of hydrocortisone sodium succinate via IV, plus 50 mg diphenhydramine via IV—is administered.
Ordering providers are required to place a note indicating that the benefits of contrast use for that particular case outweigh the risks, in addition to a notation acknowledging the limited data related to short regimens of pre-medication.
Anesthesiology and/or the department’s airway are alerted and put on standby in case cardiac or respiratory complications occur.
Once all the aforementioned boxes are checked, the patient can be given contrast and the exam can be completed, but they will remain under close surveillance to monitor for signs of delayed reactions after the scan is done.
The written protocol was distributed throughout the radiology, neurology and emergency departments, and residents and providers were educated on the steps to ensure that everyone was aware of the processes. Considering the rarity of these specific cases, there have been limited opportunities to enact the protocol. However, experts involved in its development maintain that it reduces delays in care.
“By establishing this algorithm, we can help reduce the time between stroke patient arrival and work up, which can often be delayed by a history of prior contrast allergy,” the authors suggested. “And by engaging radiologists in the imaging plan of these unique cases, we ensure that ACR contrast administration guidelines are implemented and imaging is appropriate, safe, and efficient.”
Learn more about the team’s work here.