AI needle-path generation slashes insertions times for CT-guided biopsies
Lesion detection and path planning for CT-guided biopsy could benefit from the help of artificial intelligence-based needle guidance.
Use of these assistive tools could significantly reduce puncture times without sacrificing accuracy, offering measurable improvements compared to freehand techniques that often hinge on user experience. Such improvements were detailed Jan. 21 in a new analysis in the Journal of Vascular and Interventional Radiology.
“Precise needle placement is a critical step in ensuring successful CT-guided percutaneous interventions. Although needle insertion occurs primarily in the axial plane, an out-of-plane trajectory is occasionally required to establish the safest anatomical pathway,” Tatsuya Kawai, with the Department of Radiology at Nagoya City University Graduate School of Medical Sciences in Japan, and colleagues explain. “However, performing needle insertions using freehand manual techniques is generally challenging and requires experience.”
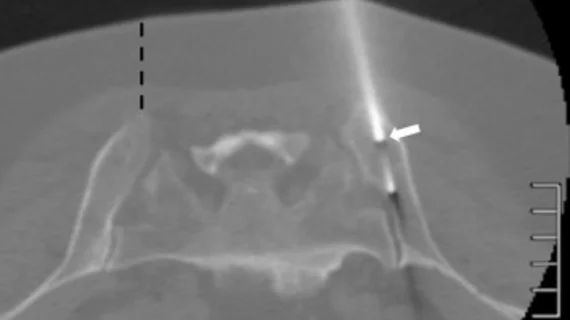
The team deployed an automated system designed to plan needle trajectories and orient needle guides using CT imaging alongside an AI-based lesion detection software for their phantom study. The phantom included eight nodules, along with simulated spinal bones and ribs.
Two groups of interventional radiologists—one with five years or more of experience and one with less than five years—completed 96 robot-assisted insertions, plus an additional 32 fluoroscopy-guided freehand insertions to compare each technique’s accuracy and time to completion. Post-insertion CT scans were used to make the comparisons.
The automated system successfully detected all phantom lesions and generated optimal needle paths. Compared to freehand methods, robot-assisted needle insertions demonstrated significantly lower depth deviations, but no difference was noted in lateral deviations. Perhaps the most substantial benefit of the AI- and robot-assisted insertions was the large reduction in insertion time, with the assisted methods taking 17.3 ± 7.8 seconds on average compared to 78.6 ± 38.1 seconds for freehand.
There are several patient care benefits of reduced insertion time, including reduced risk of pneumothorax and tissue damage owed to unexpected patient movements, the group noted. This also helps spare IRs from additional radiation exposure.
It is important to note that use of the robotic system requires an additional 20 minutes of setup time. This should be considered alongside its benefits for departments looking to incorporate the technology into their workflows.
“In recent years, numerous robotic systems have been developed, and efforts have been made to evaluate their utility,” the group notes. “However, as a challenge in robotics research within interventional radiology, it is desirable to establish metrics that enable comprehensive and reliable comparisons, not only in terms of targeting accuracy but also with respect to autonomy, ease of use, and anatomical adaptability.”