25% of patients undergoing transthoracic needle biopsy experience complications
Up to one-quarter of patients who undergo transthoracic needle biopsy experience complications post-procedure, according to new work published in the Journal of the American College of Radiology.
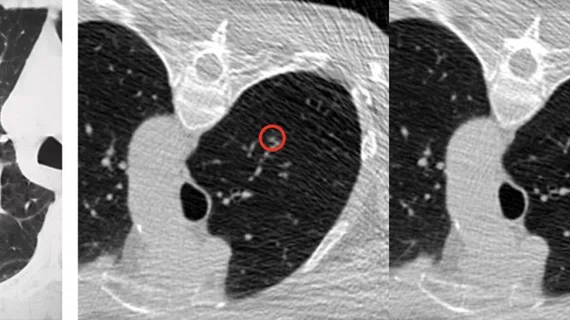
Experts analyzed more than 16,000 procedure records of patients who underwent transthoracic needle biopsy (TTNB) in 2017 or 2018 to evaluate the incidence rate of complications and how procedure settings and demographic/clinical characteristics impact adverse outcomes. Through this, they found that 25.8% of patients included in the research had experienced a complication—pneumothorax being the most common among them—within 3 days of their procedure. This led to 6.9% of outpatients being hospitalized within 7 days.
Given that TTNB is such a commonly used procedure to rule out malignancy of pulmonary nodules, experts involved in the study stressed that understanding complication rates in the midst of technological and clinical advancements is crucial to providers who are making clinical decisions that are in the best interest of their patients.
“It is unknown if complication rates have changed over time due to evolving clinical practice patterns, technological improvements, or changes in patient selection,” corresponding author Anil Vachani, MD, Associate Professor of Medicine, Division of Pulmonary and Critical Care at the University of Pennsylvania Perelman School of Medicine, and co-authors wrote. “A better understanding of the contemporary rates and patterns of complications with TTNB and factors that predispose patients to these complications can be used by clinicians and patients to make decisions on the approach to lung biopsy.”
Among the 16,971 patients who underwent TTNB, complication rates were as follows:
Pneumothorax: 23.3%
Hemorrhage: 3.6%
Air embolism: .02%
Higher complication rates were observed in inpatient settings and in patients with COPD. Also associated with increased adverse events were prior lung cancer screening and the use of oral anticoagulants or antiplatelets. Out of those with pneumothorax, 31.9% required chest tube drainage.
“The choice of biopsy approach needs to carefully weigh the diagnostic accuracy and the safety profile of the procedure itself. To minimize the complication risk and optimize the diagnostic yield, future studies are needed to determine the best practice to customize the biopsy approach based on patient’s risk group for lung cancer,” the authors concluded.
View the full study here.
More on interventional procedures:
Gadolinium can be used as substitute for iodine contrast in some interventional imaging procedures
Off-label use of WEB device effective for sidewall aneurysms
Less work, more stress—how interventional radiology departments felt the impact of COVID
Minimally invasive interventional radiology procedure delivers relief to OA patients