MRI scans deliver value as a primary screening tool for prostate cancer
MRI scans may provide value as a primary screening tool for prostate cancer, even independent of traditional prostate-specific antigen (PSA) tests, according to new findings published in BMJ Oncology.[1]
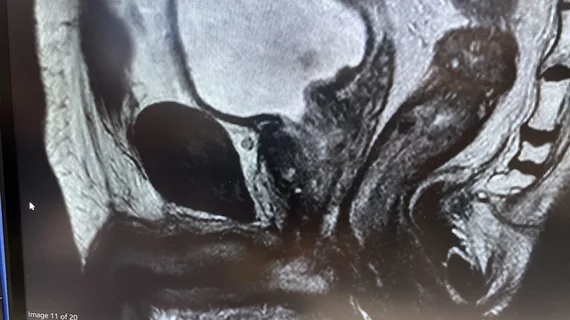
Typically, a PSA test with results at a level of 3ng/ml or above is the benchmark for performing additional tests, such as biopsies, to look for prostate cancer. Researchers sought to find out if an MRI could more accurately identify potential cancers, and if an MRI alone could be used in the future when other tests may not be available.
Looking at men most at risk (those aged 50 to 75 years old), the study's authors aimed to evaluate the prevalence of prostate abnormalities in a selected group of 2,096 patients from eight general practices in London. Participants were invited for both a screening MRI and a PSA test. While 22% responded to the invitation, and 14% completed both screenings.
The study's findings revealed that 16% of participants had a positive screening on an MRI, while only 5% had an elevated PSA density alone. Of the patients with a positive screening on an MRI, 10% had lower PSA levels than 3ng/ml, meaning they would not have received further tests for prostate cancer.
The authors pointed out that MRI scans can detect significant lesions before PSA levels rise, potentially leading to the detection of cancers that may not become clinically relevant during a patient's lifetime.
“In clinical practice, we recognize that the PSA test has limitations in the identification of men at risk for prostate cancer,” wrote lead author Caroline Moore, with the division of surgery and interventional science at University College London, and colleagues. “MRI may allow us an alternative way to assess prostate cancer risk in men in the community.”
Men in the study with an MRI that potentially showed cancer or an elevated PSA density (≥0.12 ng/mL^2) were recommended for further assessment through the National Health Service (NHS) for prostate cancer.
Study results impacted by age, race, and Covid-19
The study began before the COVID-19 pandemic, which impacted the results, since in-person visits to providers was discouraged. As a result, the researchers said the pandemic's impact on screening outcomes warrants further investigation to understand the true response rate. Respondents were also disproportionately older (aged 65-70), and it was challenging to recruit Black men for the study, despite having a higher risk for prostate cancer than white men.
“Older men were more likely to respond to the invitation, and multivariable logistic regression showed that Black men had one-fifth the response to invitation compared with white men,” the authors wrote. “Not all men who responded to the invitation were able to take part, as funding limited the number of available MRI slots, and men were allocated on a ‘first come, first served’ basis.”
The disproportionate response comes despite the ethnicity of invited men accurately reflecting the distribution across London. The researchers agree these results require further investigation, given all of the above limitations.
“The study we report here allowed us to explore the prevalence of MRI lesions in men based on age, not PSA. This knowledge will permit us to both model the performance of an MRI-based screening strategy and design the next stage in exploring its role as a primary screening test,” the authors wrote.