PSMA PET/CT shows promise for spotting metastatic disease in patients with renal cell carcinoma
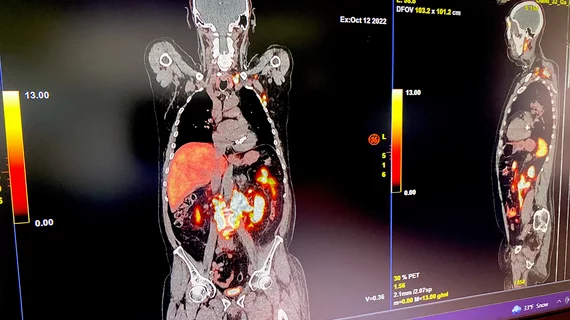
PSMA PET/CT imaging could be a more accurate alternative for staging renal cell carcinoma (RCC), according to a new meta-analysis published in the Journal of Nuclear Medicine. [1]
RCC accounts for approximately 90% of renal malignancies, but due to delayed presentation of symptoms, many people are not diagnosed until their cancer has spread. Up to 30% of patients have metastatic disease by the time they are initially diagnosed with RCC, making accurate staging a critical element of treatment planning.
The gold standard for diagnosing and staging RCC is 18F-FDG PET/CT, although this method is less sensitive to the presence of early metastatic lesions. As such, experts have been exploring other modalities in search of techniques that can more ably detect signs of early metastases.
RCC tumors are known to express prostate-specific membrane antigen (PSMA) in their neovasculature. This has prompted experts to study PSMA-targeted PET/CT imaging in patients with RCC to determine whether it might offer a better alternative for catching disease spread earlier.
For this study, experts examined nine studies on the utility of PSMA PET imaging in patients with RCC. This included a total of 152 patients with clear cell RCC (ccRCC) and other RCC subtypes and analyzed the effectiveness of two different PSMA-targeted radiotracers in detecting metastases.
The pooled detection rate of PSMA PET/CT in evaluation of primary or metastatic RCC was around 0.83, while a subgroup analysis showed a rate of 0.74 in staging or evaluation of primary RCC lesions and 0.87 in restaging of metastatic or recurrent RCC.
For radiotracers, 68Ga-based PSMA tracers yielded a detection rate of .85, while 18F-DCFPyL (Pylarify) PET/CT reached .92, respectively. In metastatic ccRCC, 18F-DCFPyL PET/CT had a significantly higher detection rate in comparison to other modalities.
“Our meta-analysis showed the detection potential of PSMA PET/CT in staging primary RCC lesions and restaging metastatic or recurrent RCC,” Moe S. Sadaghiani, MD, with the Russell H. Morgan Department of Radiology and Radiological Science at Johns Hopkins University School of Medicine, and co-authors noted. “Although our findings are based on small-scale studies with high heterogeneity, the preliminary results suggest merit in the use of PSMA PET/CT in RCC, particularly when performed for restaging of metastatic or recurrent disease.”
The authors called for larger prospective studies to confirm their findings before integrating their recommendations into clinical settings.
The study abstract is available here.