PSMA PET/CT tops conventional imaging for pinpointing high-risk cancer
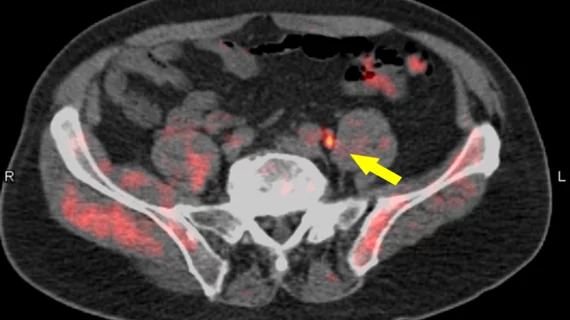
Prostate-specific membrane antigen PET/CT is more accurate than conventional imaging for pinpointing certain prostate cancers and should be incorporated into routine clinical workup.
That was the argument made by Australian researchers in a March 22 study published in the Lancet. In a trial of more than 300 men with high-risk cancer, the team found that PSMA PET/CT was nearly one-third more accurate than standard medical imaging at locating the disease.
Lead author Michael Hofman, MBBS, with the Peter MacCallum Cancer Center in Melbourne, said the findings are enough for him to suggest an addition to the currently approved pathways for men with the disease.
"Taken together, our findings indicate that PSMA PET/CT scans offer greater accuracy than conventional imaging and can better inform treatment decisions,” Hofman said in a statement. “We recommend that clinical guidelines should be updated to include PSMA PET/CT as part of the diagnostic pathway for men with high-risk prostate cancer."
There will be further analyses needed to determine the economic feasibility of widespread PSMA PET/CT use, but the researchers think such an approach could help tailor treatments on a per-patient basis.
For their randomized controlled study, Hofman et al. wanted to find out if molecular imaging could help physicians better understand how severe the disease is at a patient’s initial diagnosis.
To do so, they recruited 339 men with aggressive prostate cancer from 10 Australian healthcare institutions for their research. Each patient was randomly assigned to receive either the standard conventional CT and bone scans (152 individuals) or PSMA PET/CT (148 patients). After this, the men switched imaging protocols and received exams different from their baseline tests. One exception to this was if a patient had more than three areas of cancer spread on their first scan.
According to the results, PSMA PET/CT was “much more accurate” than CT and bone scans at detecting cancer metastasis (92% compared to 65%). This was primarily due to its ability to spot smaller sites of tumor spread, the authors wrote.
Additionally, the molecular imaging combination provided fewer false negative results and a smaller number of ambiguous results compared to the conventional approach. PET/CT also led to changes in 28% of treatment plans as opposed to 15% imaged using CT and bone scans.
Senior author of the research Declan Murphy, also with Melbourne’s Peter MacCallum Cancer Center, pointed out that one in three prostate cancer patients will relapse after surgery because current imaging couldn’t identify the disease in multiple areas of the body.
“Our findings suggest PSMA-PET/CT could help identify these men sooner, so they get the most appropriate care,” Murphy said in a statement.