CMS coverage decision for Alzheimer's drug, related PET scans sparks concern in imaging community
The Medical Imaging and Technology Alliance (MITA) recently expressed their displeasure with the Centers for Medicare and Medicaid Services (CMS) coverage decision regarding access to diagnostic testing and treatment of Alzheimer’s Disease.
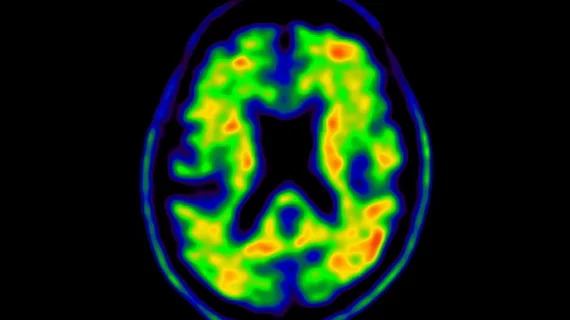
In a statement released on April 14, the alliance cautioned that the coverage decision will “severely limit patient access” to amyloid PET diagnostics and anti-amyloid monoclonal antibodies treatment. The limited access they were referring to pertains to the final CMS determination that restricts coverage of PET nuclear imaging and monoclonal antibodies directed against amyloid. The final determination states that coverage with evidence development (CED) will be granted only to those who are enrolled in CMS-approved clinical studies.
“Limiting coverage to randomized controlled trials (RCTs) for the existing FDA-approved mAB will significantly restrict and delay access for patients and families,” said Patrick Hope, executive director of MITA. “Removing the hospital outpatient-only requirement is one of the only positive changes in the final decision. Limiting amyloid PET scans to the outpatient setting would have exacerbated already severely restricted patient access due to existing Medicare payment policy.”
The Monoclonal Antibodies Directed Against Amyloid for the Treatment of Alzheimer’s Disease national coverage determination came after CMS considered more than 10,000 stakeholder comments and 250 peer-reviewed documents. Before the final determination was made, many prominent organizations in the medical imaging community, such as MITA, the American College of Radiology (ACR) and the Society of Nuclear Medicine and Molecular Imaging (SNMMI), had publicly advocated for expanded coverage, citing the benefits of beta-amyloid PET scans.
In addition to MITA calling for CMS to expand coverage eligibility to all Medicare beneficiaries, they also support removing the clause that limits coverage to no more than one scan per lifetime. Evaluating patients for therapy requires up to date diagnostic information, the statements said. This means using scans from years ago does not reliably inform clinical decisions on whether to start, stop or resume treatments.
“It is unjustifiable to predetermine that an entire class of therapies, including future FDA-approved products, is not reasonable and necessary. With more therapies becoming available, it is increasingly important to ensure the appropriate patients are identified and placed on these therapies,” said Hope. “CMS must immediately and fully cover, and appropriately pay for, FDA-approved diagnostic amyloid PET in the hospital outpatient setting.”
Read the entire MITA statement here.
Related Nuclear Imaging Content:
New radiotracer that detects prostate cancer recurrence produces 'stunning' results
Prominent imaging society advocates for 5 changes following CMS amyloid PET payment decision
Is PET/CT or multiparametric MRI best for detecting prostate cancer? New research offers guidance
F-18 FDG PET/CT highly sensitive for diagnosing cause of fevers with unknown origin