PHOTO GALLERY: thyroid nodule imaging
This is a collection of radiology imaging showing various presentations of thyroid nodules. The gallery is designed to help understand the types of imaging and procedures performed to detect, diagnose and treat thyroid nodules. Guidelines follow a grading classification system based on the way nodules appear in medical imaging. This helps determine if it is benign or cancer.
Nodules are tracked over time with imaging to watch for growth. Ultrasound and MRI can be used to show the presence of vessel formation and blood flow within a nodule, which often indicates cancer. Needle biopsies are used to take cells out of the nodule for microscope evaluation by pathology, which can identify various types of cancers, or to confirm it is benign. Nodules are often incidentally detected when patients undergo imaging exams for other purposes.
Hover over images for the caption and click on the image to make it larger.
Illustration showing the location of the thyroid in the neck and a nodule of cancer growth. The background shows a pathology microscope image of the tissue extracted from the thyroid during a needle biopsy that is used to determine if a nodule in benign or cancerous. If malignant, these images help determine cancer type.
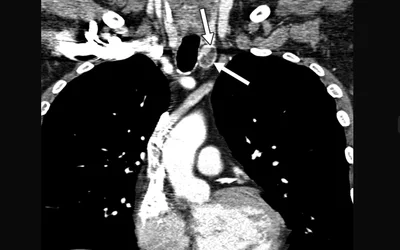
MRI angiography showing contrast enhancement of a hyperplastic thyroid nodule (arrows) in a 38-year-old man. The brain is at the top and clearly shows the aortic arch in the chest and the carotid arteries in the neck. It shows the presence of peripheral hyperenhancement of the nodule on this arterial phase image. AJR image
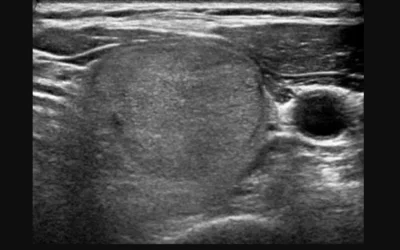
Image shows 2 cm isoechoic solid thyroid nodule without any suspicious ultrasound features, diagnosed as nodular hyperplasia by surgery. This nodule is classified as category TR3 (mildly suspicious) according to American College of Radiology (ACR) guidelines, but is a low-suspicion category according to American Thyroid Association (ATA). RSNA image
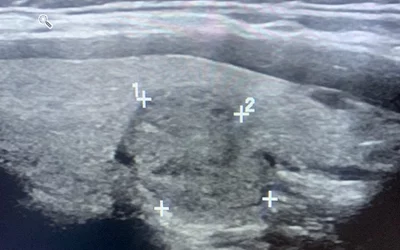
Followup Sagittal ultrasound image of the same benign nodule measuring 2 cm. This complex solid and cystic lesion is a Thyroid Imaging Reporting and Data System (TI-RADS) 3 nodule, which was recommended for ultrasound follow-up at 12 months for monitoring. It was biopsied three years prior to these images. Images used with patient permission.
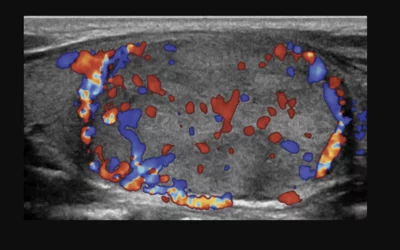
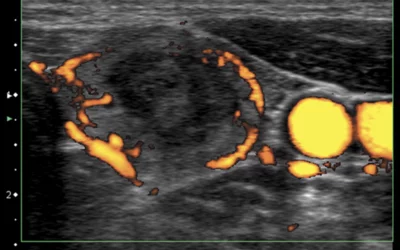
Longitudinal color Doppler ultrasound image shows increased central and peripheral vascularity in a follicular variant of papillary carcinoma thyroid nodule in a 14-year-old male. RSNA photo
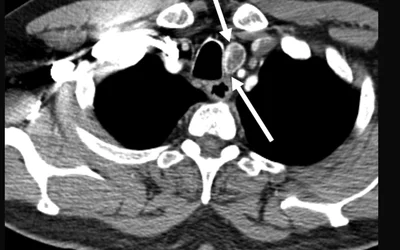
Incidental contrast-enhanced CT image of thyroid nodule in a 62-year-old man with history of lymphoma involving the parotid gland. CT was ordered to evaluate for other sites of disease. Nodule is 1.9 cm (arrows) in left thyroid lobe. AJR photo
Incidental contrast-enhanced CT image of thyroid nodule in a 62-year-old man with history of lymphoma involving the parotid gland. CT was ordered to evaluate for other sites of disease. Nodule is 1.9 cm (arrows) in left thyroid lobe. AJR photo
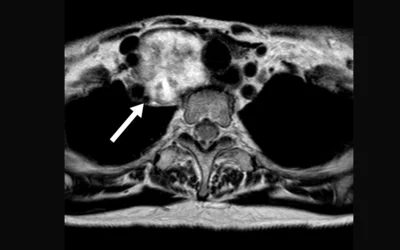
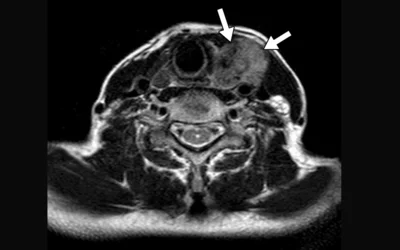
MRI image of a 66-year-old woman with papillary thyroid carcinoma. Axial T2-weighted image shows small mass located in left thyroid lobe (arrows) slightly hyperintense to abutting sternocleidomastoid muscle. AJR image
Incidental thyroid nodule finding in a 28 year-old woman undergoing a chest CT for evaluation of thoracic outlet syndrome. Contrast-enhanced axial with 5 mm slice thickness image shows a 7 mm nodule in left lobe of thyroid (arrows). AJR photo
Ultrasound image shows predominantly solid left thyroid nodule with intranodular vascularity. The nodule was benign, but underwent single-session radiofrequency (RF) ablation to reduce the size to improve cosmetic appearance and symptomatic issues. Image courtesy of RSNA
MRI of a 71-year-old woman with an adenomatous goiter. Axial T2-weighted image shows large mass located in right thyroid lobe (arrow) with strong heterogeneous hyperintensity. AJR image
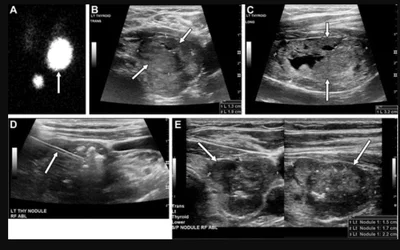
Toxic nodule in a 71-year-old woman with subclinical hyperthyroidism. (A) Iodine-123 radiotherapy thyroid uptake image demonstrates a toxic nodule in the inferior left thyroid lobe (arrow). (B, C) Ultrasound images show a corresponding nodule in the inferior left lobe (arrows). (D) Shows subtotal RF ablation of the toxic nodule, with the electrode (arrow). (E) Ultrasound acquired at 6-month follow-up shows decreased size of the target (arrows). Image courtesy of RSNA.
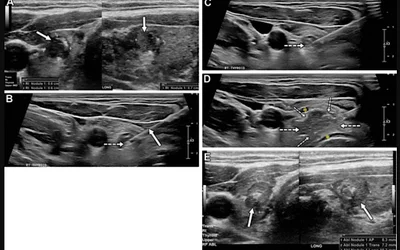
Ultrasound of a papillary thyroid carcinoma in a 41-year-old woman with hypothyroidism secondary to Hashimoto thyroiditis. (A) A high-suspicion nodule (arrows) in the right thyroid lobe. Findings from biopsy confirmed papillary thyroid carcinoma. (B, C) Ultrasound during ablation show electrode placement (solid arrow in B) in the targeted tumor and subsequent gas formation during treatment (dashed arrow). (D) Ablation zone (dashed arrows) is larger than the target lesion in cases of papillary thyroid carcinoma with use of hydrodissection to separate the trachea and strap muscles from the thyroid (*). (E) 4-month follow-up image shows expected hypoechoic area (arrows) representing ablated tissue encompassing the targeted tumor. Image courtesy of RSNA.
Pathology microscope image of biopsy showing medullary thyroid carcinoma in a 12-year-old girl with MEN-2B and bilateral thyroid nodules. High-power photomicrograph shows nests of polygonal tumor cells embedded in a dense amyloid stroma, with focal calcification. (Hematoxylin-eosin [H-E] stain; original magnification, x100). RSNA image
Pathology microscope image of biopsy showing thyroid follicular carcinoma in a 17-year-old female adolescent. High-power photomicrograph shows that the tumor invades a capsular lymphovascular space (arrows). (H-E stain; original magnification, x400). RSNA image
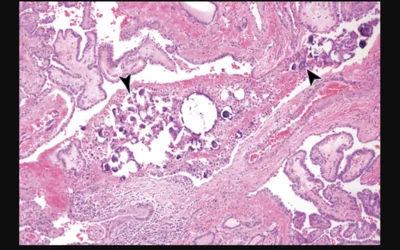
Pathology microscope image of biopsy showing thyroid papillary carcinoma in a 13-year-old female adolescent. High-power photomicrograph shows the classic type of papillary thyroid carcinoma, with central psammomatous calcifications (arrowheads). (H-E stain; original magnification, x100). RSNA image
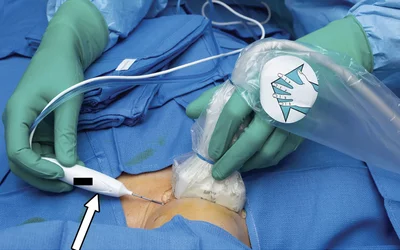
Intraprocedural image showing use of ultrasound to guide a radio frequency ablation electrode (arrow) to the thyroid in a 33-year-old woman with a benign (two negative FNAs) right thyroid lobe nodule that was producing compressive symptoms. The patient lies supine with the neck extended and general anesthesia is often used. Image courtesy of RSNA.
Ultrasound-guided fine needle aspiration biopsy (FNAB) of a solid nodule with a partial peripheral halo of a follicular carcinoma thyroid nodule in a 14-year-old male A needle guide was used (linear arrangements of descending dots) to direct the aspiration needle into the lesion. The needle is the white line. Image courtesy of RSNA.
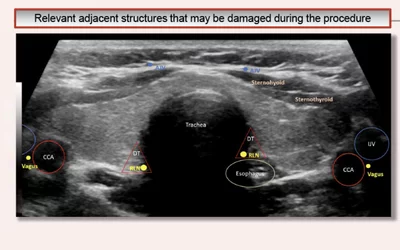
Transverse ultrasound through the thyroid at the level of the isthmus demonstrates adjacent structures that may be damaged during radio frequency ablation procedures. These include the anterior jugular vein (AJV), common carotid artery (CCA), cervical nerve (CN), danger triangle (DT), internal jugular vein (IJV), and the recurrent laryngeal nerve (RLN). RSNA image
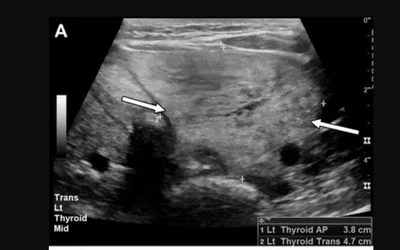
Ultrasound of a dominant left lobe nodule (arrows) in a 42-year-old woman with multinodular goiter producing compressive symptoms. Image courtesy of RSNA
Ultrasound shows RF ablation of the left lobe nodule, commencing in the superficial portion of the gland with significant shadowing deep to the ablation site (arrows), which illustrates why the deeper portions are ablated first. This necessitated a delay in further treatment until the gas disappeared. In a 42-year-old woman with multinodular goiter producing compressive symptoms. Image courtesy of RSNA
Intraprocedural ultrasound image showing the RF ablation electrode (arrow) guided to the thyroid in a 33-year-old woman with a benign (two negative FNAs) right thyroid lobe nodule that was producing compressive symptoms. Image courtesy of RSNA
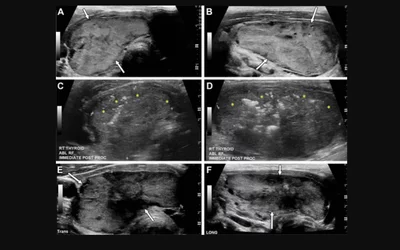
Large nodule in the right thyroid lobe causing cosmetic concerns in a 45-year-old woman. (A, B) Ultrasound shows a nodule measuring 56 × 41 × 26 mm (31 mL) (arrows). (C, D) Ultrasound acquired after RF ablation shows residual tissue in the peripheries (*). The initial response showed a decrease of 30% after 1 month. (E, F) Ultrasound obtained 1 year after RFA shows the nodule (arrows) has regrown and measures 58 × 38 × 22 mm (25 mL). RSNA image
Measurements on ultrasound to determine volume reduction of a radio-frequency ablation treated thyroid nodule 6 months after initial RF ablation. Image courtesy of RSNA
Moving shot technique from deep (1) to superficial (3) in a biopsy-proven papillary thyroid cancer in a 41-year-old woman. Moving shot technique describes the repositioning of the electrode in multiple subunits, moving from superficial to deep. This ensures adequate coverage of the nodule while avoiding over treatment of the peripheries. Note the club-shaped ablation zone (red shading) that should overlap on subsequent ablation cycles. Knowledge of the adjacent sensitive structures is important, in particular the recurrent laryngeal nerve in the “danger triangle” (blue outline). Image courtesy of RSNA.
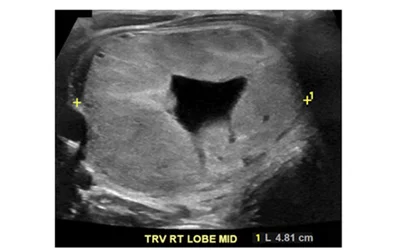
There has been criticism of the American College of Radiology (ACR) TI-RADS reporting criteria because it may be inadequate for younger populations, as a high percentage of cancers would be missed when looking at pediatric thyroid nodules. This example shows a 16-year-old with a thyroid follicular carcinoma on ultrasound. The 4.8 cm isoechoic, smooth nodule with no echogenic foci would be a TI-RADS 2, which under the reporting criteria recommends no follow-up. Image courtesy of RSNA
There has been criticism of the American College of Radiology (ACR) TI-RADS reporting criteria because it may be inadequate in younger populations, as a high percentage of cancers would be missed when looking at pediatric thyroid nodules. Sagittal ultrasound of 18-year-old female with papillary thyroid cancer shows a 4.8-cm thyroid nodule that is mixed cystic and solid and isoechoic, with smooth margins and no echogenic foci (TR2). ACR TI-RADS criteria recommended no fine-needle aspiration biopsy or follow-up. Image courtesy of RSNA
There has been criticism of the American College of Radiology (ACR) TI-RADS reporting criteria because it may be inadequate for younger populations, as a high percentage of cancers would be missed when looking at pediatric thyroid nodules. This is an example of a 13-year-old girl with subcentimeter papillary cancer appearing as a 0.7 cm thyroid nodule that is solid and hypoechoic, with irregular margins and echogenic foci (TR5). TI-RADS recommended follow-up, but not fine-needle aspiration biopsy because of the nodule’s size of less than 1 cm. Image courtesy of RSNA
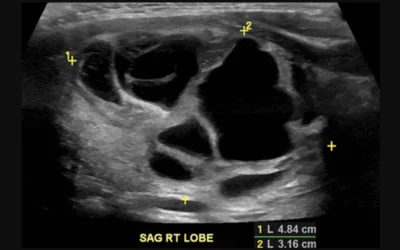
Whole-body SPECT scintigraphic image showing the ghostly image of the patient's faint body outline from the radiation they are emitting. The image shows thyroid papillary carcinoma in this 58-year-old man six days after administration of 4.52 GBq radioactive Iodine-131 sodium iodide. It shows up as a large black area in the neck. The thyroid has an affinity for iodine, so radioactive iodine is often used to treat the organ. RSNA image
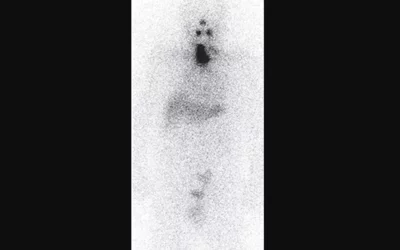
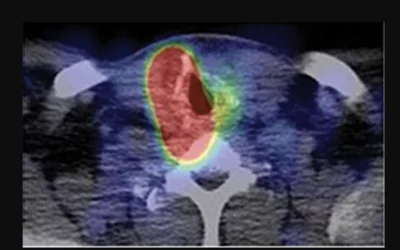
SPECT/CT fusion images show radioactive iodine accumulation in the residual thyroid remnant of thyroid papillary carcinoma in a 58-year-old man 6 days after administration of 4.52 GBq radioactive Iodine-131 sodium iodide. The colors show the intensity of the radiation being emitted. RSNA image
Related Content:

Dave Fornell has covered healthcare for more than 17 years, with a focus in cardiology and radiology. Fornell is a 5-time winner of a Jesse H. Neal Award, the most prestigious editorial honors in the field of specialized journalism. The wins included best technical content, best use of social media and best COVID-19 coverage. Fornell was also a three-time Neal finalist for best range of work by a single author. He produces more than 100 editorial videos each year, most of them interviews with key opinion leaders in medicine. He also writes technical articles, covers key trends, conducts video hospital site visits, and is very involved with social media. E-mail: dfornell@innovatehealthcare.com














![Pathology microscope image of biopsy showing medullary thyroid carcinoma in a 12-year-old girl with MEN-2B and bilateral thyroid nodules. High-power photomicrograph shows nests of polygonal tumor cells embedded in a dense amyloid stroma, with focal calcification. (Hematoxylin-eosin [H-E] stain; original magnification, x100). RSNA image](/sites/default/files/styles/gallery/public/2025-02/pathology_medullary_thyroid_carcinoma_in_a_12-year-old_girl_rsna.png.webp?itok=22eWTyCk)



















![<p>Pathology microscope image of biopsy showing medullary thyroid carcinoma in a 12-year-old girl with MEN-2B and bilateral thyroid nodules. High-power photomicrograph shows nests of polygonal tumor cells embedded in a dense amyloid stroma, with focal calcification. (Hematoxylin-eosin [H-E] stain; original magnification, x100). <a href="https://pubs.rsna.org/doi/abs/10.1148/rg.2017170059">RSNA image</a></p><p> </p> Pathology microscope image of biopsy showing medullary thyroid carcinoma in a 12-year-old girl with MEN-2B and bilateral thyroid nodules. High-power photomicrograph shows nests of polygonal tumor cells embedded in a dense amyloid stroma, with focal calcification. (Hematoxylin-eosin [H-E] stain; original magnification, x100). RSNA image](/sites/default/files/styles/teaser/public/2025-02/pathology_medullary_thyroid_carcinoma_in_a_12-year-old_girl_rsna.png.webp?itok=wTAWgUAM)





![<p>Moving shot technique from deep (1) to superficial (3) in a biopsy-proven papillary thyroid cancer in a 41-year-old woman. Moving shot technique describes the repositioning of the electrode in multiple subunits, moving from superficial to deep. This ensures adequate coverage of the nodule while avoiding over treatment of the peripheries. Note the club-shaped ablation zone (red shading) that should overlap on subsequent ablation cycles. Knowledge of the adjacent sensitive structures is important, in particular the recurrent laryngeal nerve in the “danger triangle” (blue outline). <a href="https://pubs.rsna.org/doi/full/10.1148/rg.22002]\">Image courtesy of RSNA.</a></p> Moving shot technique from deep (1) to superficial (3) in a biopsy-proven papillary thyroid cancer in a 41-year-old woman. Moving shot technique describes the repositioning of the electrode in multiple subunits, moving from superficial to deep. This ensures adequate coverage of the nodule while avoiding overtreatment of the peripheries. Note the club-shaped ablation zone (red shading) that should overlap on subsequent ablation cycles. Knowledge of the adjacent sensitive structures is important, in particula](/sites/default/files/styles/teaser/public/2025-02/moving_shot_technique_to_reposition_rf_ablation_electrode_to_treat_thyroid_lesions_rsna.jpg.webp?itok=NQ7NvXiy)