Common cancer screenings may not lead to longer lives, with 1 key exception
Early detection is touted as the number one way to improve cancer outcomes, but a new study out of Norway is calling into question established wisdom regarding routine screenings, particularly for lung and breast cancer. The findings were published in JAMA Internal Medicine. [1]
Lead author Michael Bretthauer, MD, PhD and his team discovered that, while it’s assumed screening is linked to a longer life following a cancer diagnosis, that “fact” is not always backed by current evidence. However, that does not mean he and the other researchers are calling for an end to screenings.
“Although our meta-analysis suggests that claims that screening saves lives are not substantiated by the current best available evidence, we do not advocate that all screening should be abandoned,” Bretthauer and colleagues wrote. “Screening tests with a positive benefit-harm balance measured in incidence and mortality of the target cancer compared with harms and burden may well be worthwhile.”
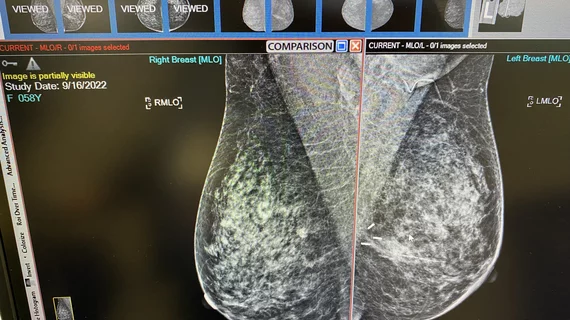
The study encompassed data from a total of 2,111,958 participants from 18 randomized clinical trials. The analysis covered various cancer screening methods, including sigmoidoscopy and fecal testing for colorectal cancer, PSA screening for prostate cancer, CT lung cancer screening for smokers, mammography screening for breast cancer, and colonoscopy screening for colorectal cancer. The study also incorporated a trial that explored the cumulative impact of multiple cancer screening tests on lifetime gain.
The outcomes were mixed. Sigmoidoscopy emerged as the sole screening method associated with statistically significant life extension, quantified at an average of 110 days, with a range spanning from zero to 274 days. In contrast, mammography yielded no additional days of life gained.
The results for CT scans for lung cancer come in at an average of 107 days, but there’s a catch: The spectrum of days of life gained extended from a potential loss of -286 days to a gain of 430 days. In other words, researchers could not conclude there was any benefit from a CT lung screening.
The researchers noted that the lack of substantial life extension might be attributed to a multitude of factors.
“Due to the stigma and the psychological burden, a cancer diagnosis may also cause extra noncancer-specific deaths from suicide, cardiovascular disease, and accidents," they wrote. "Also, increased surveillance after cancer screening may increase the risk of other incidental disease, which would not have been detected without screening."
Bretthauer et al. also acknowledge that early-stage cancer detection and treatment can indeed improve mortality rates, especially at a young age. However, they propose that screenings should be weighed against a balanced assessment of benefits vs. harms, measured in terms of cancer incidence, mortality rates, and associated burdens, and not just conducted arbitrarily.
“However, organizations, institutions, and policymakers who promote cancer screening tests by their effect to save lives may find other ways of encouraging screening,” the authors wrote. “It might be wise to reconsider priorities and dispassionately inform interested people about the absolute benefits, harms, and burden of screening tests that they consider undertaking. Our estimates may serve that purpose.”
The full story can be found here.