4 key trends in breast imaging
As women's imaging centers emerge from the COVID era of the past three years, here is a list of key breast imaging trends to consider. These are trends observed by the editors of Health Imaging and discussed by some of the experts in mammography.
These trends include:
• Rapid movement toward 3D mammography
• Growth of supplemental imaging for women with dense breasts
• A growing role for artificial intelligence
• Compounding issues from lower reimbursements
There were more than 39.6 million breast exams performed in 2022, according to the U.S. Food and Drug Administration (FDA) Mammography Quality Standards Act (MQSA) program, which inspects breast imaging facilities and certifies each imaging system. As of January 2023, the FDA said there are 8,808 certified U.S. breast imaging facilities and more that 24,500 accredited mammography systems.
3D mammography is becoming the new standard of care
The biggest trend in mammography is the change in bread-and-butter imaging technology. Full-field digital mammography (FFDM) has been the standard modality for breast imaging for about two decades, but digital breast tomosynthesis (DBT) systems, also known as 3D mammography, are seeing rapid growth and are replacing FFDM.
As of January 2023, the FDA's MQSA statistics show DBT systems now make up 46% of mammography systems in the U.S. About 1,000 new tomo breast imaging systems are added each year according to the FDA stats, meaning DBT will likely replace the vast majority of FFDM mammography systems within the next decade.
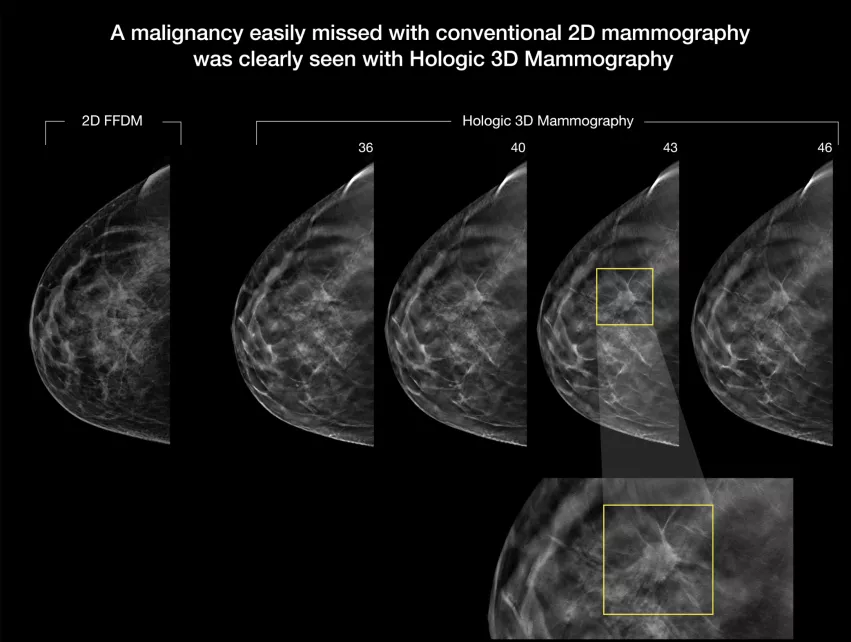
Breast imaging centers are adopting the newer 3D mammography technology because it has the ability to view the breast in slices, similar to a CT scan. This allows areas that appear to have a mass to be viewed layer by layer to see if the suspicious area is just overlying layers of dense breast tissue. Users say this helps a lot in determining if a patient should be called back for additional imaging, biopsy, or if the area of concern is just overlapping tissue.
"From my experience, tomosynthesis is now the default breast imaging modality. I suspect there are still some centers doing only full-field digital mammography, but I think they are far and few between," explained Society of Breast Imaging (SBI) President John Lewin, MD, associate professor of radiology and biomedical imaging, and division chief, breast imaging, at the Yale School of Medicine.
He said a lot of centers still have FFDM systems, but they are using their newer DBT systems as their front-line imaging workhorse systems. Certainly at the larger academic centers and breast centers he has worked with in recent years for referrals, he is receiving DBT datasets to review.
"We are excited about 3D tomosynthesis, where we can do thin slices through breast tissue to uncover these cancers that hide in those dense, dense areas of the breast," said Constance "Connie" Lehman, MD, PhD, chief of breast imaging, co-director of the Avon Comprehensive Breast Evaluation Center at the Massachusetts General Hospital, and professor of radiology at Harvard Medical School.
Initially, adoption of DBT was low because there was no reimbursement, but that has changed, making it easier for centers to justify the expense of these systems.
"We went from several years ago where very few facilities or hospitals had one unit, to now where we have facilities completely converting over to tomosynthesis. So the implementation has been pretty wide over a quick period of time," explained Stamatia Destounis, MD, FACR, a radiologist and managing partner at Elizabeth Wende Breast Care in Rochester, New York, chair of the American College of Radiology (ACR) Breast Commission, and member of the Public Information Advisors Committee for Radiological Society of North America (RSNA) and SBI Communication Committee.
For more, watch the VIDEO: The rapid adoption of 3D mammography and use of AI to address dense breasts.
A comparison between 2D and 3D mammography on the Hologic Selenia Dimensions Mammography System. 3D tomosynthesis shoots a series of images of the breast can can be flipped through as slices of specific layers of the breast tissue, where 2D shows all the breast tissue in one image. Dense breast tissue can hide cancers, as can be seen here where one of the 3D slices found a cancer masked by dense tissue on the 2D image.
"There are several benefits to this, and the number one benefit is a reduction in call back rates, so women are not getting called back for false alarms and false positives," Destounis explained. "That really makes life easier and reduces the workload for the radiologist so we don't have to focus so much time on calling patients. We also have an increased cancer detection rate. With tomosynthesis we get a better mammogram where we can find more cancers and reduce patient anxiety. It is just a better test and I do think it will continue to have wide implementation."
While DBT technology is better at detecting more cancers and reducing false positives, it also comes with a much larger number of images to review, increasing the time it takes to read these exams. The larger datasets means radiology departments need much larger data storage capability.
"Even though it is more time-consuming to read the tomosynthesis screenings, it is becoming the standard-of-care. And I have to say, there is extra reimbursement if you do a mammography and a tomosynthesis, and that definitely has had an effect on adoption," Lewin said.
The standard for diagnosis is still 2D mammography. This is partly because the majority of prior exams used to compare changes in breast tissue between exams are still used. Regulators wanted true apples-to-apples comparisons, but this is hard to do with a 3D mammogram. This could require the patient to undergo a standard 2D mammogram and then the 3D exam, increasing the amount of radiation they receive and the overall costs.
However, Destounis said this issue has been solved by vendors programming their 3D systems to create a synthetic 2D mammogram view.
Increasing use of supplemental imaging for women with dense breasts
For women with dense breasts, it is difficult to detect cancers because the dense tissue appears as white on mammograms, and so do cancers. Lewin said dense tissue can mask smaller cancers, so these women may need supplemental breast screening with breast ultrasound, contrast enhanced mammography or breast MRI. The public campaigns to raise awareness about dense breasts and advocacy efforts to get breast density inform laws on the books in many states have helped increase the use and reimbursement for supplemental imaging.
An increased number of cancers that were not identified through mammography in women with dense breasts can be found using breast ultrasound. However, it is a relatively small number of additional cancers. Adding in breast MRI or vascular imaging can lead to a huge leap in finding new cancers.
"Using screening ultrasound in addition to mammography, we will find two additional cancers per 1,000 women on average, and that is on top of the three to four we typically find from mammography alone," Lewin explained. "That is fine, but if you add contrast-enhanced breast MRI, you increase that number to 15-19 more cancers. Most of these additional cancers will be invasive and identified because of the cancer's increased blood supply. And with MRI, it is not really finding more cancers, we are just finding cancers earlier when they are smaller and more easily treated."
While MRI is very effective, it is has a longer exam time, is more expensive and it is not always covered by insurance.
"We know that if we screened everyone using MRI we would save more lives, but we have never proven this in a randomized trial. So what we do instead is to screen women at higher risk using MRI, and we know anecdotally that we do find cancers that we would not have found for years using standard methods," Lewin explained.
Adding in breast MRI or vascular imaging can lead to a huge leap in finding new cancers. Vascular imaging of the breast can be performed with both MRI and contrast-enhanced mammography. Lehman said contrast enhanced mammography can show areas of dense vascular growths that are generally associated with cancer. She said the technology holds a lot of promise, because it can be used with existing mammography systems, but the technology needs to show its efficacy evidence in clinical trials.
"I would say if you have a patient who is at risk for having a cancer missed on mammography, look to vascular imaging and MRI," Lehman explained. "But we also know MRI is rife with problems. Patients are uncomfortable with the MRI, it is costly [and] we don't have access to high-quality breast MRI in all regions. And that is why I think the future is so bright for contrast-enhanced mammography."
Existing mammography systems can be upgraded to perform contrast mammo exams, so she believes this will help offset issues with access to MRI. It also can be performed at the same imaging center where patients get their breast screenings, so it does not require scheduling additional appointments at other locations.
"I believe from the early data from the first studies that have come out, that contrast-enhanced mammography is going to perform very well compared to contrast enhanced MRI at a fraction of the cost," Lehman said. "It also would be a significant bump up for women having access to the technology."
There are currently reimbursement issues with contrast-enhanced mammography, but she said with additional clinical evidence, this will change over time. That additional clinical evidence will come partly from the new, large-scale Contrast-Enhanced Mammography Imaging Screening Trial (CMIST). Being conducted in partnership with the ACR, the Breast Cancer Research Foundation and GE Healthcare, the study launched in the fall of 2022.
Read more:
Contrast-enhanced mammography to get rigorous tryout under ACR’s oversight.
VIDEO: Why contrast enhance mammography might be the ideal supplemental imaging
VIDEO: Use of supplemental imaging in women with dense breasts
Role of AI in mammography
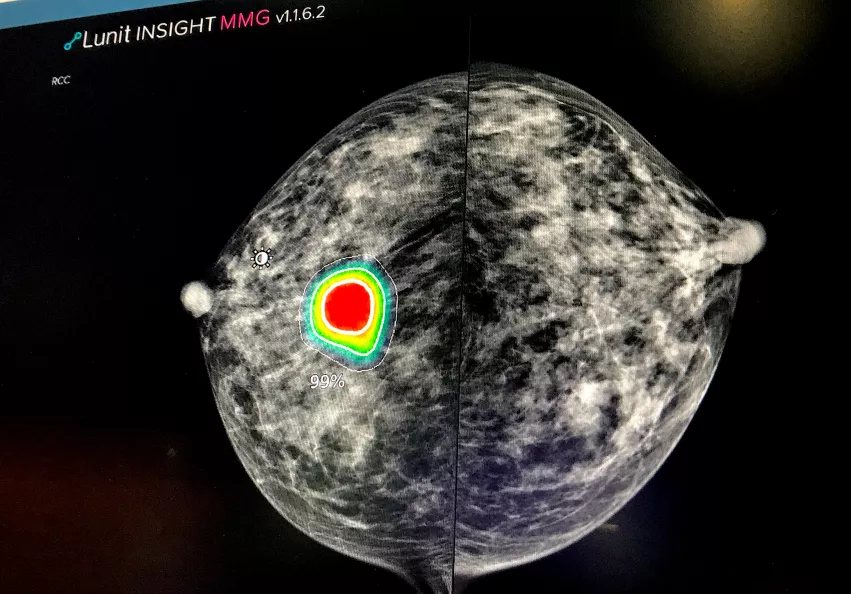
FDA-cleared artificial intelligence (AI) algorithms are being implemented in breast imaging to help augment radiologists. This includes automated assessment of breast density that removes inter-reader variability, and automated scanning of all breast images for the detection of areas of interest that may include suspected cancers.
"I think AI is still in its relatively early phase of adoption," Lehman said. "We do have some centers that are not academic centers that are very forward thinking and really wanting to bring AI into their practices. However, we are also seeing a story that is very familiar when we are bringing computer-aided detection (CAD) into both academic and community centers. The technology is being incorporated into clinical care, but we are still studying what the actual outcomes are on patients who are being screened with mammography where AI tools are or are not being used."
AI for automated detection of breast cancer lesions and flagging these as areas of interest on mammograms can help radiologists know where to pay closer attention. AI also can take a first pass look at mammograms to determine if they appear to be normal, so radiologists can prioritize which exams need to be read first and which may be more complex.
This technology will likely become more important as the number of breast imaging exams switches over from traditional four-image mammogram studies to much larger 3D digital breast tomosynthesis (DBT) exams of 50 or more images. AI is already being used to flag images that deserve a closer look in these datasets at some centers, which can help speed reading times.
"Artificial intelligence is playing a role here, fine tuning areas of interest for us to look at," Destounis said. "There may be a role for AI to help radiologists, but we certainly are not saying AI will replace the breast radiologists. The early AI studies show AI can accurately predict risk for the patients based on the breast parenchymal patterns seen on the mammogram. I think there will be a role for AI to help act as a second set of eyes and to concentrate on these women that may be considered high risk based on their parenchymal pattern or some risk score that is assigned by AI."
However, the most exciting area of AI for breast imaging is in the potential of radiomics, where the AI will view medical imaging in ways that human readers cannot to identify very complex and small patterns. These patterns will help better assess patient risk scores, or what the best outcomes will be based on various cancer treatments.
"What I am really excited about is the domain where investigators are considering the power of artificial intelligence to do things that humans cannot or are not very good at, and then to allow the humans to really focus on those tasks where humans excel. As of today, these AI tools have not even really scratched the surface," Lehman explained.
She said this area of research using radiomics moves beyond training AI to look at images like a human radiologist and to instead pull out details that are usually hidden from the human eye. This includes rapid computer segmentation and analysis of the morphology of disease or tissue patterns seen in images, looking for minute regional structures that can be detected by AI and looking at thousands or hundreds of thousands of data points in the image.
"This is not to train AI to look at mammograms like I do, but to train the AI to look for patterns and signals that my human eyes and human brain cannot detect or process," Lehman said.
For more:
VIDEO: The rapid adoption of 3D mammography and use of AI to address dense breasts
VIDEO: Role of AI in breast imaging with radiomics
Lower reimbursements and higher costs impact the bottom line of breast imaging
Lower reimbursement is seen as big issue by all three of the experts we interviewed. They agreed lowering payments for breast imaging is one of the biggest barriers to improving care, adopting new technology and retaining and attracting radiologists for breast imaging jobs.
Destounis said the exams and procedures at her outpatient center are reimbursed less than hospitals, which takes a toll. "For the same procedures, we may be reimbursed at a lower rate than a hospital, including breast ultrasound, stereotactic needle biopsy and breast MRI."
While reimbursements are going down, the costs for biopsy systems, markers and MRI contrast are all going up. In addition, because of supply chain disruptions since the start of COVID-19, many supplies are often delayed or on backorder for long periods, she said.
The reach of the "Great Resignation" into radiology has also been partly fueled by lower reimbursements, which has made it difficult to attract experienced radiologists.
Reimbursements are also a driver for which imaging modality is used. If the case of FFDM and 3D DBT, if a reimbursement is the same, but DBT systems cost more, there is less incentive to buy the new technology.
"If you had a community that was really having challenges in resources, would you rather screen twice as many women with 2D mammography, or screen half as many women with 3D?" Lehman said.
She added this is exactly the type of decision many rural or lower-income area centers are making.
This was exactly the finding the a study published in Radiology in October 2022, which highlights the relationship between race and access, or lack thereof, to evolving mammographic screening techniques.[1]
The paper, which focused on 4 million Medicare claims 2005 to 2020, revealed that Black women had less access to newer mammographic technology than their white peers, even when their exams took place within the same institution. Although cancer detection rates among Black and white women are similar, Black women are 40% more likely to die from breast cancer, in part, due to the stage at which their cancer is detected—an occurrence that is inevitably impacted by access to newer screening technology, authors of the study suggested.
“Inequities result when lower payments make technology investments economically unsustainable for practices that serve higher proportions of Medicare patients,” explained study co-author Eric W. Christensen, PhD, principal research scientist in health economics for the Harvey L. Neiman Health Policy Institute.
The payments Christensen is referring to are Medicare reimbursements dictated by the Centers for Medicare and Medicaid Services (CMS). Private insurers offer reimbursements 1.2 to 1.8 times higher than public insurers such as Medicare, which exacerbates healthcare disparities in underserved areas where many utilize public insurance.
According to the new data provided by Christensen and colleagues, although these gaps in care do appear to soften over time, this does not occur at an equitable pace.
“Current reimbursement contributes to inequity because locating new technology in facilities that serve patients with public insurance, Medicare and Medicaid, is not economically sustainable,” Christensen said. “CMS can create economic incentives to lessen disparities through reimbursement that is either comparable to private payers or that more directly incentivizes adoption of newer technology in underserved communities.”
Read more:
'Economically unsustainable': How Medicare reimbursements hinder adoption of latest mammo technology.
VIDEO: Issues with the great resignation and lower reimbursements in breast imaging