AI quantifies breast arterial calcifications on mammograms
A new artificial intelligence tool can fill in reporting gaps related to breast arterial calcifications (BACs) identified on mammograms.
Though the association between BACs on breast imaging and cardiovascular disease among women was once a highly debated topic, numerous recent studies have provided additional evidence supporting the link between the two. Despite this, there are no standards requiring radiologists to report on the presence of BACs, even though up to half of referring providers have indicated they would prefer to be made aware of the finding.
Quantifying BACs on imaging would present an increase in workload for radiologists. But new research set to be presented during the American College of Cardiology's Annual Scientific Session (ACC.25) suggests that AI can help ease this burden.
"We see an opportunity for women to get screened for cancer and also additionally get a cardiovascular screen from their mammograms," the study's lead author Theo Dapamede, MD, PhD, a postdoctoral fellow at Emory University in Atlanta, said in a news release. "Our study showed that breast arterial calcification is a good predictor for cardiovascular disease, especially in patients younger than age 60. If we are able to screen and identify these patients early, we can refer them to a cardiologist for further risk assessment."
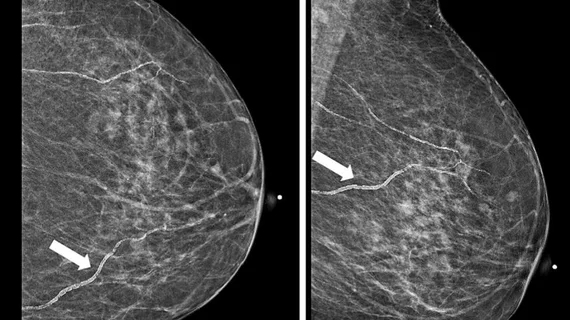
Researchers from Emory Healthcare and Mayo Clinic trained a deep learning model to segment calcified vessels on mammograms. A combination of the segmentations and data from tens of thousands of electronic medical records enables the model to calculate the risk of future cardiovascular events.
The model categorizes patients’ risk of heart attack, stroke or heart failure as low, moderate or high. It performed well in accurately predicting the likelihood of these events at two time points—two years and five years after the imaging was acquired. It also identified ages that are most at-risk, including women under 60 and between 60 and 80.
It revealed that women with the highest level of BACs were at significantly greater risk of major events and lower rates of event-free survival. The team estimates that women with higher categories of BACs are at 2.8 times higher risk of death within five years compared to those with little or no BACs.
Experts involved in its development believe the tool could be beneficial in identifying younger women who may be at greater risk of cardiovascular events, paving the way for earlier diagnoses and intervention.
ACC’s annual meeting will take place in Chicago March 29-31.