Chemical imaging method could improve radiotherapy planning
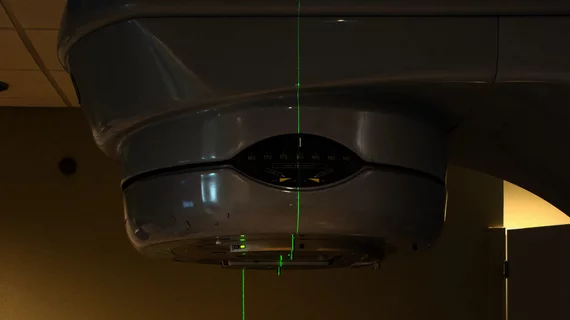
A new chemical imaging method could change how providers plan radiation therapy treatments for cancer patients [1].
Radiation therapy planning is typically based on anatomical imaging, like PET/CT and MRI, but experts recently suggested that a form of chemical imaging could better predict tumor behavior and, in turn, help clinicians to understand how tumors would respond to certain treatments.
A team of experts from the University of Michigan and two universities in Italy (University of Calabria and University of Padua) has been researching a method known as photo acoustic chemical imaging, or PACI, to understand how it can offer added insight into the chemical makeup of a tumor.
Details of the research were published recently in ACS Nano, where University of Michigan chemistry professor Raoul Kopelman, a co-senior author of the paper, and colleagues explained how the method could contribute to providers’ ability to cater treatments specifically to cancer patients’ needs.
"This would allow for optimization of treatment methods for a particular patient—precision medicine," Kopelman said.
The method injects nanoparticles into tumors to sense chemicals of biochemical interest, like oxygen, sodium and potassium, etc. An infrared laser is used to detect the nanosensors and the light then penetrates tumor tissue; this creates an ultrasound signal that is used to map the distribution of the chemical of interest within a tumor.
The research team recently deployed this method to sense oxygen in tumor tissue within mice undergoing radiotherapy. Following the radiation therapy, the group was able to use the PACI method to determine how successful the treatment was at destroying cancerous tissue, with lower levels of oxygen indicating less effective treatment.
"Such chemical mapping would help the clinical team prescribe a personalized, optimal treatment for a given patient's tumor, based on the new diagnostics from the tumor xenograft's chemical mapping,” Kopelman noted.
In terms of whether this method could be translated into radiotherapy planning for humans, Kopelman believes it can. It would require creating chemical maps in patients directly but could be achieved with fiber optics that are threaded through the venous system to come within appropriate range of the tumor. Similar methods are used in various cardiac procedures.
In order for the method to be effective in humans, nanosensors would need to be developed for each chemical of interest and each would require FDA approval, the team notes.
The study abstract is available here.