90% of breast imaging centers now offer 3D tomosynthesis
Purchases of new digital breast tomosynthesis (DBT) systems have been been rising rapidly in recent years. In fact, they now account for nearly half of all U.S. mammography imaging systems.
The latest statistics released by the U.S. Food and Drug Administration's Mammography Quality Standards Act and Program (MQSA) on Aug. 1 show DBT systems are now used in 90.5% of breast imaging centers.
DBT systems now make up 48% of mammography systems in the U.S. and will likely surpass 50% in the next year. There have been 837 new DBT systems put into service in the past year, which is nearly four times as many as the 213 new 2D mammography systems installed during the same time. The number of new 2D systems sold to U.S. facilities appears to be flat.
Experts in the field say the rising numbers of 3D mammography systems show it is becoming the new standard of care. There are 26,045 mammography systems in service in the United States according the MQSA. Of these, 13,603 are digital mammography systems and 12,442 are newer DBT systems.
Women's imaging centers are still purchasing standard 2D full-field digital mammography (FFDM) systems. This is likely because FFDM is less expensive than 3D tomo systems and the IT and reading time requirements are much lower. Tomo systems require much more digital storage capability to handle datasets that are 10 times larger or more than 2D exams. The larger number of images also take much longer to read. Some centers use their 3D systems to screen women with dense breast tissue, and others with less dense breasts are imaged on 2D systems.
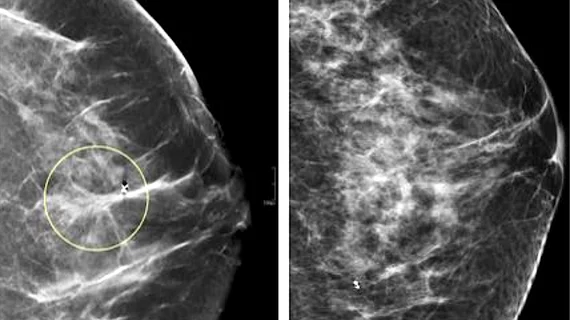
Breast imaging centers are adopting the newer 3D mammography technology because it gives radiologists the ability to view the breast in slices, similar to how CT imaging is displayed. This allows readers to view suspicious areas layer by layer to see if it is just overlapping layers of dense breast tissue or if it is cancer. Cancer and dense breast tissue look very similar on 2D mammography. Users say this helps determine whether a patient should be called back for additional imaging and/or a biopsy.
Barriers have slowed wider adoption of DBT
The first FFDM unit was approved for marketing in January 2000, and quickly became the new standard of care because of its improvements in image quality over film mammography systems. The first DBT system was cleared by the FDA in 2011. Initially, adoption of DBT was low because there was no reimbursement, but that has changed in recent years, leading to a spike in new DBT systems being purchased.
The standard for diagnosis is still 2D mammography because it is the same imaging format for the majority of prior exams used to compare changes in breast tissue between screenings. Regulators of mammography systems want a true apples-to-apples comparison of prior breast imaging to see any changes inside the breast. Early on, this required the patient to undergo a standard 2D mammogram and then the 3D exam, increasing the amount of radiation they received and costs they incur. But DBT system vendors have since added features to create a simulated 2D mammogram along with the 3D dataset to avoid the need for additional imaging.
The time to read 3D DBT exams is also longer than 2D exams. Instead of just a handful of images, the DBT datasets include 40 or more images to look through. However, artificial intelligence (AI) will likely see increasing use to help look through these exams. AI can do a first pass and flag images where radiologists should spend more time because the software detected something that was not normal.
"Standard mammogram would only be four pictures back in the days of film and early digital, but now with tomosynthesis, that same study can can involve over 200 images. Multiply that times 50, 75, or 100 cases a day, and that is a massive volume of images to look at. The good news is now there are some algorithms out there to actually reduce those number of tomosynthesis images to be reviewed," Samir Patel, MD, CCD, DABR, FACR, diagnostic radiologist at Radiology Inc. and Beacon Health System, who spoke with Heath Imaging in a video interview at RSNA 2023. He said AI assistance for 3D mammography will likely become one of the biggest use cases for AI in radiology.
He said AI can triage the exams, prioritizing reports with suspected critical findings for radiologists to review promptly. Also, many FDA-cleared algorithms can automatically perform measurements of breast lesions and assess mammograms for breast density BI-RADS scores.