5 Years into the Cloud, John Muir Health Is Just Getting Started
One 3D mammogram acquired via digital breast tomosynthesis adds about 500 MB of image data to a hospital’s storage system. That’s the average. On the high end, a single study can occupy as much as 3 GB of real estate on a finite-volume storage server.
Thought experiment: Multiply that potentiality by the thousands of patients receiving 3D mammograms every year at any given hospital or breast center.
For now, call it a three-hospital, 1,000-physician, geographically dispersed healthcare system clinically affiliated with two major academic medical institutions. Then figure in all the enterprise imaging studies the organization must obtain and store. These include not only DICOM medical images across radiology and cardiology but also photos, videos, cineloops and digitized slides from dermatology, ophthalmology, gastroenterology, pathology, wound care and obstetrics. And put that healthcare system in a region vulnerable to earthquakes, forest fires and controlled power shutoffs.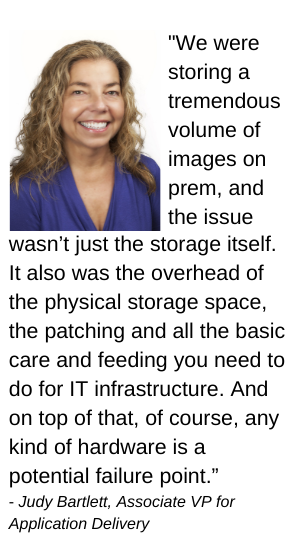
Five years ago at Walnut Creek, California-based John Muir Health—yes, it has three hospitals and 1,000 or so doctors and is dispersed across the San Francisco Bay Area—this scenario was not just a hypothetical to think through. It was a clear and present problem to solve. The organization then managed about 150 terabytes of data, which has doubled in the years since.
“We could not get our heads around the exploding growth,” recalls Enterprise Technology Architect Marty Tedlock, who now mostly focuses on the cloud. “We would have half-day exercises with white boards trying to figure out, ‘OK, how much disk space do we have to purchase to stay ahead of imaging just over the next couple of months?”
The data deluge had been building at John Muir Health for some time, he says, but it was the arrival of 3D breast tomosynthesis that made the search for a better solution urgent.
“At that point, oh my gosh, I was having heart attacks trying to figure out where I was going to put all this image data,” Tedlock says.
His colleague Judy Bartlett, Associate VP for Application Delivery, remembers the tomo-driven growth spurt coinciding with John Muir Health’s ambitious overall growth plans. The health system was adding or expanding one practice, clinic or facility after the next.
 “We were storing a tremendous volume of images on prem, and the issue wasn’t just the storage itself,” Bartlett says. “It also was the overhead of the physical storage space, the patching and all the basic care and feeding you need to do for IT infrastructure. And on top of that, of course, any kind of hardware is a potential failure point.”
“We were storing a tremendous volume of images on prem, and the issue wasn’t just the storage itself,” Bartlett says. “It also was the overhead of the physical storage space, the patching and all the basic care and feeding you need to do for IT infrastructure. And on top of that, of course, any kind of hardware is a potential failure point.”
The concern reached the top of the IT division when a storage area network indeed did fail. Tedlock recalls the CIO setting a new direction on the fly.
“We had been looking to replace dedicated storage for PACS when the SAN failed,” Tedlock remembers. “The CIO said, ‘Well, we can’t go that route anymore. We’ve got to head somewhere else altogether.’”
It wasn’t immediately apparent, but the “somewhere else” would lead them to the cloud.
Tedlock and Bartlett recently recounted their cloud journey from its first steps to the present day.
They also itemized some of the myriad benefits, quantifiable as well as experiential, that have accrued along the way.
Ideas and allies for building cloud storage for healthcare
The cloud arose as a first-line option for image data management from the foundation of John Muir Health’s longstanding relationship with Sectra, Tedlock and Bartlett explain.
More recently, in 2017, the health system tapped Sectra’s Image Exchange Portal to facilitate clinical collaboration with area care partners like UCSF Health in San Francisco and Stanford Children’s Health in Palo Alto.
Very soon after Sectra suggested John Muir Health consider the company’s primary cloud package—a software suite called Sectra Health Cloud with a licensing model called Sectra One Cloud Services—the deliberations were on.
“There was a lot of whiteboarding internally, including with hospital leadership, and we had a lot of discussions with Sectra leaders about concerns,” Bartlett says, adding that they were open to cloud but had some big questions: “Is this even a viable option? Does this really make sense? Are we going to take performance hits? Are we going to have providers screaming and yelling, ‘What have you done to us?’”
As stakeholders hashed out the plan, aims like digital footprint management, cybersecurity, and optimization of productivity and innovation emerged as high-level needs. From these flowed more tactical points of consideration. One was somewhat unique as such for John Muir Health—disaster preparedness.
Housing healthcare data away from earthquake zones using the cloud
 “On one side of the street, we’ve got the Hayward Fault and the other side is the San Andreas Fault,” Tedlock says. “Both are kind of due for a little shake. So having the core of our applications and data stored between those two faults doesn’t make good sense. Moving our applications to the cloud with a cloud-based plan for disaster recovery made perfect sense.”
“On one side of the street, we’ve got the Hayward Fault and the other side is the San Andreas Fault,” Tedlock says. “Both are kind of due for a little shake. So having the core of our applications and data stored between those two faults doesn’t make good sense. Moving our applications to the cloud with a cloud-based plan for disaster recovery made perfect sense.”
 All the more, since earthquakes aren’t the only major threats to geological normalcy in the Bay Area. Summer often brings wildfires to the area, and with fall come controlled but not always predictable blackouts and brownouts.
All the more, since earthquakes aren’t the only major threats to geological normalcy in the Bay Area. Summer often brings wildfires to the area, and with fall come controlled but not always predictable blackouts and brownouts.
The latter affected a John Muir Health data center even though it’s backed by generators, “but we don’t see the utility companies making any major changes within the next 10 years to rectify that,” Tedlock says. “That also helped settle us on Sectra Cloud, largely because of Sectra’s great reputation for reliability.”
Another key voice in that decision—yes to cloud and yes to a Sectra pathway to cloud access—came from a group of insistent end-users. “The radiologists,” says Tedlock. “They just loved Sectra from all their past experience with the company and its products. And we don’t want IT to be done to them. We want them to guide us in our IT decisions.”
Finally, John Muir Health had recently subscribed to Microsoft Office 365, which features cloud-based productivity and security components applicable across the enterprise. This meshed with Sectra’s own cloud approach, which is rooted in a close collaboration with Microsoft.
“Our information security team had already blessed the Microsoft Azure solution,” Tedlock says. “I wouldn’t say it’s a one-stop shop, but the existing Sectra-Microsoft partnership made things very simple. It carried a lot of weight into the decision of going forward with the Sectra cloud solution.”
Appreciated outcomes of medical imaging cloud storage
How does that decision look five years down the road? Going by the verifiable and still unfolding outcomes, it was the right move at the right time.
Radiology was first into the cloud. Cardiology has been on its own cloud and, if all goes according to plan, will be on Sectra Health Cloud by the end of 2022. (COVID interfered with the initial timeframe.)
W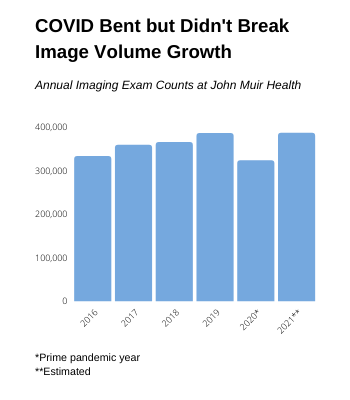 ound care is slated to begin migrating early next year, to be followed as soon as feasible by endoscopy, pathology and newly acquired specialty practices that are joining John Muir Health with their own imaging systems.
ound care is slated to begin migrating early next year, to be followed as soon as feasible by endoscopy, pathology and newly acquired specialty practices that are joining John Muir Health with their own imaging systems.
“We recently acquired a practice with 10 years of images stored,” Bartlett clarifies. “Our plan is to migrate those images to the cloud so we don’t have to maintain a separate system and take on the overhead that goes with that separate system.”
So pronounced have been the improvements of cloud usage with Sectra that Bartlett doesn’t stumble when asked to predict the long-term future of cloud-enabled healthcare.
“We’ve gotten to a point where everything is digital,” she says. “Marty and I can remember working with paper and films for a very long time. So when you start thinking about where we’ll be 10 years from now, I’d guess patients will be able to access everything in their medical records, including imaging studies and reports. And they’ll be doing it all on their own devices via an EHR in the cloud. I think transparency and portability will finally be the norm rather than the exception.”
Tedlock agrees. “First we had film. Then we went to floppy disks, then CDs, then USB drives. And now computers with ports for any external physical inputs are becoming rare. I don’t think it’s too far a leap from where we are now to a place where patients and their care teams are all sharing images, info and communications over their smartphones—or whatever replaces smartphones over the next 10 years—in the cloud.”
Bartlett and Tedlock believe that, as that first wave of 3D tomosynthesis studies hinted, healthcare providers who think they can embrace enterprise imaging while avoiding the cloud are probably in for a shock to their system well before 10 years from now. Time will tell, but their warning seems sound from the vantage point of 2021.
For more on enterprise imaging in the cloud with Sectra, click here.

