Experts suggest new follow-up imaging protocols for vaccine-related lymphadenopathy
Experts are reporting that follow-up ultrasound imaging for reactive axillary lymphadenopathy is likely not necessary before 12 weeks.
A new study published in Radiology followed 88 women diagnosed with reactive axillary lymphadenopathy after receiving a COVID vaccine for several months to monitor for changes on ultrasound imaging. Persistent lymph node swelling was observed on imaging for more than 50% of women at the 12-week mark, prompting experts to suggest this follow-up time interval as a reasonable guideline.
“As more studies with long-term data are being published and radiologists continue to gain more clinical experience, it is becoming clear that both the incidence and duration of vaccine-related adenopathy are greater than initially expected,” Dr. Linday Moy, professor of radiology at New York University and senior deputy editor for Radiology, and Dr. Eric Kim, clinical assistant professor in the breast imaging section of the Department of Radiology at the NYU Grossman School of Medicine and a Senior Deputy Editor of the Radiology In Training editorial board, wrote in an editorial alongside the article by Ha et al. “The recommendation by Ha and colleagues to increase the follow-up imaging interval from 4-12 weeks to more than 12 weeks seems reasonable to reduce the number of follow-up examinations.”
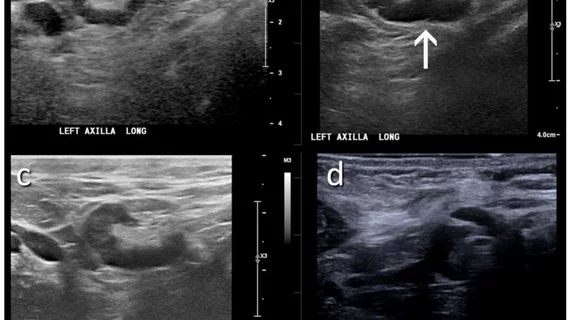
The study consisted of a cohort of 88 asymptomatic women without breast cancer who had been vaccinated against COVID and soon after developed axillary lymphadenopathy. Each woman underwent serial ultrasound imaging to monitor changes over a median period of 12 weeks. Experts assessed cortical thickness, number of lymph nodes, morphology and Doppler signal on all imaging.
Of the 88 women for whom follow-up imaging was available, complete lymphadenopathy resolution was observed in 26% at the 6-week mark. For 51% of the women, the swollen lymph nodes were still visible after 12 weeks. Notably, cortical thickness gradually decreased over time for all of the women.
“Clinicians and radiologists should understand the different timelines for lymphadenopathy resolution according to the vaccine type and cautiously interpret lymphadenopathy considering the timeframe from vaccination and overall nodal metastatic risk of individual patients,” corresponding author Jung Min Chang, MD, with the Department of Radiology at Seoul National University Hospital, and study co-authors explained. “Even in situations that require follow-up US examinations, short-term follow-up within 6 weeks is not helpful for identifying the resolution of lymphadenopathy.”
Related COVID Vaccine Adenapathy Content:
VIDEO: Should women wait to get mammograms after COVID vaccination?
How radiology providers can minimize mammography recalls among COVID-vaccinated patients
Most routine imaging should be scheduled 6 weeks after 2nd vaccine dose, major cancer centers say
Managing COVID-19 vaccine side effects: Harvard radiologists share their ‘pragmatic’ approach
COVID-19 vaccine update: Radiologists report side effects mimicking breast cancer on mammograms
Women do not need to delay their mammogram appointment after COVID-19 vaccination.
Molecular imaging group shares updates for managing COVID-19 vaccine effects on PET/CT exams
Radiologists report COVID vaccine side effects mimicking breast cancer on mammograms
These ultrasound features distinguish between COVID vaccine-related and malignant adenopathy
Related Ultrasound Content:
O-RADS externally validated for differentiating between benign and malignant ovarian lesions
Algorithm performs at expert level when distinguishing between benign and malignant ovarian tumors
Specialized ultrasound can accurately detect prostate cancer, new research shows
These ultrasound features distinguish between COVID vaccine-related and malignant adenopathy