Experts use MRI to identify brain pathways responsible for epileptic seizures
Researchers recently used a series of MRI brain scans to identify pathways in the frontal lobe that could be the root cause of some epileptic seizures.
Sharing their findings in Brain, experts involved in the work suggested that the results of their analysis could help guide neurosurgery in patients with seizures that do not respond to medication, potentially eliminating their seizures in the long-term.
A team of researchers at the UCL Queen Square Institute of Neurology in London came to this conclusion following their retrospective assessment of 47 cases of patients who had undergone prior neurosurgery to their frontal lobe as a means of treating their epilepsy. The patients’ MRI scans were used alongside their subsequent follow-ups to identify similarities on imaging among those who responded most favorably to surgical treatment.
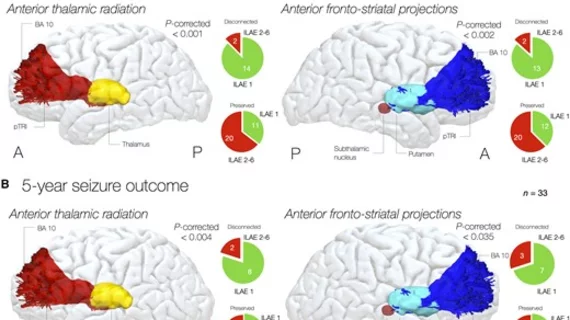
The team found that those who had pathways between their frontal lobe and thalamus and striatum (the anterior thalamic radiation and anterior cortico-striatal projections, specifically) disconnected recorded the most marked seizure-free time periods, with 88% of patients being seizure-free after three years and 80% remaining seizure-free after five years.
Lead author of the study Davide Giampiccolo, a neurosurgeon with the UCL Queen Square Institute of Neurology and Cleveland Clinic London, and colleagues explained what led them to investigating these pathways:
“As thalamic and striatal dysregulation can support epileptogenesis and disconnection of cortico-thalamostriatal pathways through hemispherotomy or neuromodulation can improve seizure outcome regardless of focality, we hypothesize that projections from the striatum and the thalamus to the cortex may contribute to this common epileptogenic network,” the team noted.
What’s more, the surgical disconnection of these pathways did not negatively affect the patients’ language or executive functions, the team shared, later adding that, if proven true, this finding could have a great impact on surgical outcomes for patients with epilepsy.
“This will allow us to redesign neurosurgical operations and personalize the operations for each patient, ensuring that the right connections are cut. We hope this will lead to a great improvement in the long-term results of epilepsy surgery.”
The detailed research is available here.