No need for updated imaging prior to major surgery in some cases, new data show
Prior chest imaging can sometimes be just as predictive of adverse events after surgery as updated imaging, according to new data set to be presented at the annual conference of the American College of Cardiology (ACC) on March 5.
It is common for patients who are undergoing major surgery to require cardiac clearance beforehand due to the increased risks of heart attack, stroke and other adverse events that such operations pose. Often, this clearance will entail some form of chest imaging, but if there is available imaging already on hand from prior exams that occurred within a 12-month window, this additional imaging may not be necessary to appropriately gauge risks, experts involved in the new study suggest.
“Our findings show that imaging already on hand can help physicians make practical decisions about surgical risks, even though such tests may not be as precise as those designed for this purpose,” said lead author Daniel Choi, MD, a cardiology fellow at NYU Langone Health.
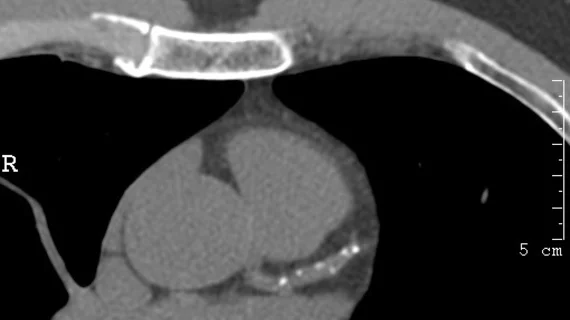
For the study, experts analyzed the EHR data of 2,650 patients ages 45 and older who underwent surgery between 2016 and 2020 for non-cardiac reasons. Each patient also had completed a chest CT scan within one year of their surgery. Experts recorded instances of heart attacks and death with available data from the CT scans to understand whether providers with no formal training in imaging could accurately correlate the presence of coronary calcium with patients’ risks.
Providers completed a 90-minute training session on estimating coronary calcium severity based on imaging. They then used a scoring system to grade calcium severity in the heart’s three major coronary arteries for the patients included in the research, ranging from 0-9 and “absent” to “severe.”
Patients with scores of 0 to 2 were found to have a 4% or lower risk of major adverse cardiac events (MACE); those with 3 to 5 had an 8% risk, which increased to 13% for scores of 6 to 9. These estimates were consistent among all physician participants.
The team highlighted the simplicity of the system, noting its efficacy across each provider after the 90-minute training session. They suggest that although the use of prior imaging might not be quite as precise as updated exams, it could be a cost-effective, suitable alternative that saves time and avoids additional radiation exposure to patients.
To learn more, click here.