7 COVID vaccine complications: The radiologist's role in identifying adverse reactions
Although adverse events related to COVID-19 vaccines are rare, some are life-threatening. Due to the radiologist’s important role in identifying vaccine reactions, it is important that they are familiar with how complications present on imaging.
With the onset of the pandemic and vaccine rollout now well in the rearview mirror, experts have gained much knowledge about the effect of COVID vaccines. Common side effects include pain at the injection site, low-grade fever, headache and fatigue, but these are all temporary and typically subside within a few days.
More worrisome are the rare adverse effects some individuals experience, some of which can have dire consequences. A new paper in Clinical Imaging provides a thorough overview of documented vaccine complications and details the radiologist’s role in identifying them before they become life-threatening.
The multi-organ complications are categorized and described below:
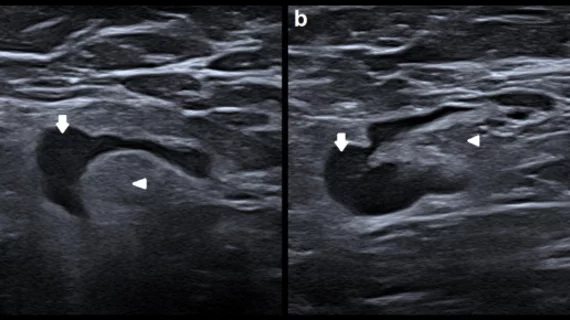
Lymph node complications. Lymphadenopathy is probably the most common adverse side effect on the list. Though it is fairly common and inconsequential for most, it can complicate interpretations of exams on patients with a history of lymphoma, breast cancer and head and neck cancer, as reactive lymphadenopathy most often occurs in the axillary, supraclavicular and cervical regions. These areas are where the aforementioned cancers typically metastasize. When these findings are present, it’s important that radiologists are made aware of patients’ vaccine history, including if, when and what type of COVID vaccine they received.
Vascular complications. Coagulopathy is also a known complication of COVID vaccines, though this more often occurs with viral vector vaccines, with much fewer reported after an mRNA vaccine. Vaccine-induced immune thrombotic thrombocytopenia (VITT) can cause venous and arterial thrombosis, including cerebral venous sinus thrombosis (the most serious), pulmonary embolism and deep vein thrombosis. If symptom onset occurs within 5–30 days after vaccination, patient has thrombocytopenia, a positive D-dimer and PF4 antibodies, the presence of clots is likely reactive, the authors suggested. Depending on the area of concern, patients should undergo ultrasound, CT or MRI, but for urgent cases involving neurological symptoms, the group suggests referring patients for an urgent non-contrast CT head and CT venogram, or an urgent MRI of the head and contrast enhanced MR venogram.
Cardiac complications. Cases of myocarditis and myocardial infarction following mRNA vaccines were among some of the earliest adverse events reported. It is estimated that myocarditis has occurred in approximately 1.62% of vaccine recipients. Chest pain and high cardiac enzymes shortly after COVID inoculation, especially with an mRNA vaccine, could indicate an adverse vaccine reaction, the group suggested. In terms of imaging, Adding T1 mapping, T2 mapping and extracellular volume to the routine CMR can help characterize the disease.
Neurological complications. Neurological adverse events outside of headache and dizziness are rare, though there have been reports of severe neurological complications like acute transverse myelitis, acute disseminated encephalomyelitis, Bell's Palsy, Neuromyelitis Optica Spectrum Disorder, Guillan-Barre syndrome, stroke and seizures. These are more common following second vaccines. CT and MRI can both be used when post-vaccine neurological complications present, though MRI is the preferred modality. Radiologists should pay attention for hypersensitivities on FLAIR sequences, T2 signal alteration in the spinal cord, T2 and gadolinium enhancement of the caudal nerve roots, and enhancement of the distal intra-canalicular and labyrinthine segments of cranial nerve 7 and the geniculate ganglion on contrast enhanced T1-w MRI.
Pulmonary complications. One of the more serious post-vaccine complications that has been reported is radiation recall pneumonitis (RRP). This occurs in patients who have previously undergone radiation therapy to the lungs or have undergone other treatments (chemo, immunotherapy, cancer drugs, etc.) for lung cancer. On imaging, this presents similarly to radiation pneumonitis. Patients will present with acute dry cough, shortness of breath and low-grade fever. The timing of previous cancer treatment is important in determining whether RRP is reactive. CT is the modality of choice for this complication. Common image findings include ground-glass opacities and air space consolidation limited to the radiation field.
Abdominal complications. Abdominal pain, nausea, vomiting, diarrhea, and dyspepsia are common during the first day or two after COVID vaccination. The most common serious adverse event post-vaccine is appendicitis.
Renal complications. Minimal change disease (MCD), IgA nephropathy, antineutrophil cytoplasmic autoantibody vasculitis and acute interstitial nephritis have all been reported shortly after receiving the vaccine, though MCD is the most common. Imaging referrals should be based on patients’ symptoms, but ultrasound, CT or MRI could all be appropriate.
“Although these complications are severe and potentially life-threatening, they are rare, and the benefit of the vaccine supersedes the risks,” corresponding author Nanditha Guruvaiah Sridhara, with the Department of Radiology at Wake Forest University Baptist Medical Center, and colleagues noted. “It is important for radiologists to be aware of these potential complications and the associated imaging findings so that they can make a prompt diagnosis and allow for improved patient management.”
The group stressed the importance of radiologists being informed on patients’ vaccine history, including the type and timing of the shot.