Interventional radiologist completes first procedure in US using new embolectomy system
An interventional radiologist at Staten Island University Hospital just aided in the first endovascular procedure in the United States that utilized new technology designed to improve outcomes in cases of acute pulmonary embolism.
Vincent Gallo, MD, director of vascular and interventional radiology, completed the procedure alongside the hospital’s Chair of Cardiology Mitchell Weinberg, MD. The duo was the first in the U.S. to use Jupiter Endovascular Inc.’s Endoportal Control platform technology—part of the company’s Vertex Pulmonary Embolectomy System.
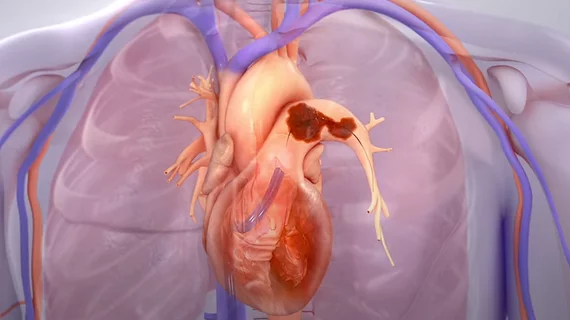
The platform was developed to improve the complex, often time-consuming process of navigating through pulmonary arteries during embolectomy procedures. Integrated into the Vertex system, it enables providers to treat areas that are typically more difficult to reach using conventional endovascular techniques.
“Navigating the pulmonary arteries can be challenging and often requires a complex trial-and-error approach involving multiple guide wires and ancillary devices in order to safely reach the target vessels,” Gallo said in a release. “Using Endoportal Control with the Vertex system, we eliminated many of these extra steps and device exchanges, resulting in a much simpler procedure that allowed us to focus less on gaining vessel access and more on treating the patient.”
The procedure marks the first in the U.S. of the SPIRARE 2 clinical trial—a prospective, single-arm, multicenter trial that will test the utility of the embolectomy system at 25 sites. The trial’s endpoints will characterize the clinical and procedural benefits of the system and monitor side effects, safety, heart function and improvements 30 days post-procedure.
The first U.S procedure to utilize the system was successful, Jupiter CEO Carl J. St. Bernard shared.
“Navigation challenges during endovascular procedures are often underappreciated and have led to under-adoption of life-saving procedures, such as pulmonary embolectomy. We have purpose-built our Endoportal Control technology to solve these issues and make important endovascular procedures accessible to more clinicians and their patients who can benefit from them,” St. Bernard said. “This first case in the U.S. could not have gone better, and appears to validate the safety and performance we are seeing in our currently enrolling European SPIRARE I study.”
Learn more here.