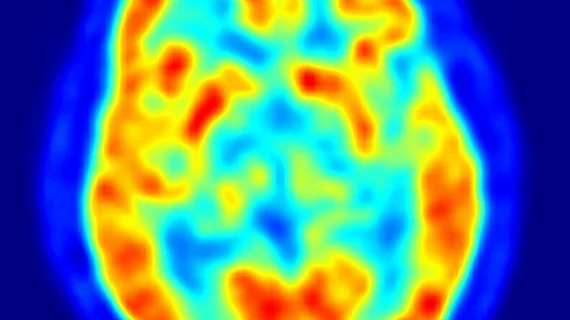
PET study shows promise for treating lethal brain cancers
Johns Hopkin’s researchers have created a PET-based approach that can direct cancer drugs to precise points in the brains of mice, according to a study published in the May 1 edition of the Journal of Nuclear Medicine.
If proven effective in humans, the researchers believe their technique could help patients with difficult brain tumors, such as glioblastomas.
“Cancer drugs are often administered as pills or intravenous injections, which are easy and comfortable for patients, but only a tiny portion of these drugs reach the brain tumor. Most of it accumulates in other organs, often leading to serious side effects,” said co-author Piotr Walczak, MD, PhD, with Johns Hopkins University School of Medicine, in a prepared statement. “The intra-arterial approach solves this problem by allowing us to deliver highly concentrated treatments directly and selectively to the tumor.”
Their technique employs a method traditionally used to treat strokes which involves guiding a catheter from an artery in the leg, through the body and into the brain—intra-arterial delivery—and combines it with PET scanning to pinpoint drug delivery.
In the study, the researchers compared intra-arterial and intravenous injection with and without opening the blood-brain barrier in three separate mouse cohorts.
The first involved four healthy mice in which researchers used the drug mannitol to open the blood-brain barrier. They delivered a standard dose of the radiotracer bevacizumab, labeled Zirconium 89 via the catheter and scanned the mouse brains using PET imaging for 30 minutes after drug delivery, one hour and one day after treatment.
A second group of four mice received the same intravenous treatment without opening the blood-brain barrier and were imaged at the same time intervals.
The final group of four mice received the same amount of bevacizumab intravenously and underwent PET imaging 15 minutes before mannitol opened their blood-brain barrier, then 30 minutes, one hour and one day after treatment.
Of the three experiments, intra-arterial drug delivery with an opened blood-brain barrier was the best as 23.58% of the dose per cubic centimeter reached the brain, staying there 24 hours after the treatment.
“Although a little more technically demanding than the standard intravenous approach, the degree of enhancement of antibody uptake within the brain using the intra-arterial approach could revolutionize antibody-based immunotherapy for neurooncology,” said co-author Martin Pomper, MD, PhD, a professor in the Johns Hopkins radiology department, in the same statement.