Imaging Addiction: Could PET & MR End Cocaine Abuse?
Cocaine addiction can ruin a person physically and financially, and with an estimated 1.4 million cocaine users in the U.S., thousands will become trapped by their habit. While previous research on the drug and its addictive potential were observational and subjective, imaging is reshaping how we see addiction—and how it will be treated.
“Neuroimaging [functional and structural MRI, pharmacological MRI, PET] has made a huge contribution to our understanding of cocaine dependence, as it helped us to elucidate the neurobiological substrates of [addiction] and how these underpin clinical symptoms and disrupt cognitive function,” explains Karen D. Ersche, PhD, of the University of Cambridge in the U.K. Ersches’s research focuses on psychopharmacology and addiction.
Addiction studies have not always utilized imaging in this manner. In the past, when researchers wanted to investigate cocaine addiction, they had to rely mainly on observing an animal test subject’s drug-seeking behavior or hear a subjective description of a “high” from a human subject. Both methods are limited.
“It is considered in some ways reliable, but it is not really explaining the mechanisms by which [cocaine] is working,” says Shankar Vallabhjosula, PhD, of Weill Cornell Medical College in New York City. “Showing where in the brain it binds and what happens to the dopamine levels, that is our real objective.”
PET offers a powerful neuroimaging technique to quantify the binding of neurotransmitters in the brain. One of these neurotransmitters, dopamine, is the key to understanding addiction. Cocaine modifies the action of dopamine in the brain by binding to dopamine re-uptake transporters on the pre-synaptic membrane. Dopamine-rich areas in the ventral tegmental area, the nucleus accumbens and the caudate nucleus—the brain’s “reward pathway”—are responsible for the positive feelings that come from certain stimuli. By inhibiting the ability of transporters to remove dopamine and increasing activation of the reward pathway, cocaine causes users to feel high and euphoric.
Getting Worse with Age Losing Gray Matter |
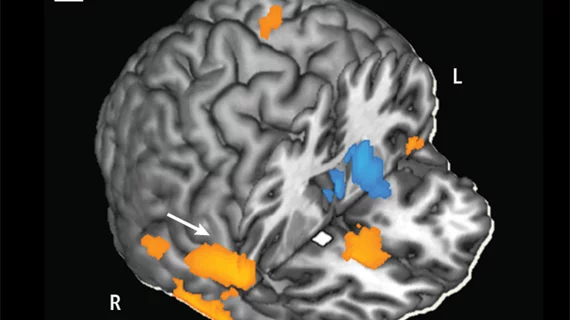
In addition to cocaine's potential for overdose and negative behavioral changes, it also leads to a reduction of gray matter volume most commonly associated with aging. That was the conclusion from Karen D. Ersche, PhD, of the University of Cambridge, and colleagues in a 2012 study published in Molecular Psychiatry. The study featured 120 adults between the ages of 18 and 50, half of whom met the criteria for cocaine dependence. Based on structural MRI scans of the subjects' brains, Ersche and colleagues found the annual rate of global gray matter volume loss in cocaine-dependent individuals was 3.08 milliliters per year, nearly twice the rate of the healthy volunteers. Cocaine-addicted individuals had declines in the prefrontal and temporal regions in particular, and experienced brain changes in their 30s and 40s more commonly seen in people over 60. "If cocaine-dependent individuals age faster than their biological age suggests, this should have implications for treatment," says Ersche. "Healthcare professionals need to take into account that a cocaine or crack user in his mid-40s may have greater levels of cognitive decline than one would expect from a normal person of the same biological age. For clinical practice, this would require adjustments in the way in which information is communicated to people with a history of chronic cocaine abuse." |
Treatment-seeking behavior
Vallabhjosula and colleagues are now devoted to using molecular imaging and fresh insights into cocaine addiction to test a vaccine that can help addicted individuals quit. The vaccine, developed by Weill Cornell researcher Ronald G. Crystal, MD, is based on a cocaine analog linked to the proteins of a serotype 5 adenovirus. It is designed to evoke anti-cocaine antibodies that trap cocaine in the blood and prevent it from affecting the brain.
The researchers used PET imaging with the tracer 11C-PE2I to measure cocaine occupancy in the dopamine transporter of primate test subjects before and after vaccination. They found that before treatment, cocaine occupancy was 62 percent, but after vaccination, the animals demonstrated occupancy levels of less than 20 percent—well below the 47 percent threshold required to evoke a subjective high.
“By looking at an imaging study, one can easily tell if somebody is taking cocaine or not, or if the vaccine is working or not working,” says Vallabhjosula, who adds that studies being planned now will look at human subjects to determine how many times the vaccine must be administered to be effective.
Another potential treatment comes not from blocking cocaine with a vaccine, but from normalizing brain activity and connectivity in the regions affected by addiction. Methylphenidate, commonly used to treat attention deficit hyperactivity disorder, also has demonstrated an ability to improve brain function in cocaine users, says Rita Z. Goldstein, PhD, of the Icahn School of Medicine at Mount Sinai Hospital in New York City.
Using resting-state functional MRI, another arrow in the quiver of addiction imaging researchers, Goldstein, lead author Anna B. Konova, MA, and colleagues from the U.S. Department of Energy’s Brookhaven National Laboratory in Upton, N.Y., and Mount Sinai demonstrated methylphenidate’s ability to strengthen connectivity between brain regions involved in regulating emotions and exerting behavior control, while simultaneously decreasing connectivity between areas of the brain involved in the formation of habits. The effect was strong enough to, at least transiently, change abnormal connectivity in cocaine users when compared with healthy subjects.
Previous studies also have shown the drug’s benefits with regard to keeping cocaine users engaged in cognitive tasks because it can enhance the salience of environmental stimuli. “We want to use this property, but we want to increase the salience of the right stimuli,” says Goldstein. “We don’t want to increase the salience of drug-related cues, for example.”
The main advantage of methylphenidate is that it works similarly to cocaine in that it blocks the dopamine transporter, but does so with slower pharmacokinetic activity. Where cocaine takes 20 minutes to reach peak effects, methylphenidate can take as long as 90 minutes, reducing the drug’s addictive potential, according to Goldstein.
Next steps in cocaine brain research
Currently, there’s no FDA-approved treatment for cocaine addiction, but modern neuroimaging techniques are making it easier to test potential treatments and better understand the correlation between a cocaine high, cravings and related drug-seeking behaviors and brain function in real time. “While a person is actually experiencing a high, we can see that the people with more of a dopaminergic reaction to the drug experience a more intense high,” explains Goldstein. “However, with chronic use, the dopaminergic reaction and function at baseline are markedly reduced.”
These kinds of techniques could have implications in the treatment of addictions beyond cocaine, says Vallabhjosula. “The imaging technique we have established with [the 11C-PE2I radiotracer] is really not only to assess cocaine addiction, it can assess any kind of addiction that people have because they all work through the same mechanism of dopamine high.”