AI model outperforms rads at distinguishing malignant from reactive lymph nodes on US
An artificial intelligence model recently proved more accurate than breast radiologists at differentiating between malignant and vaccine-related lymphadenopathy.
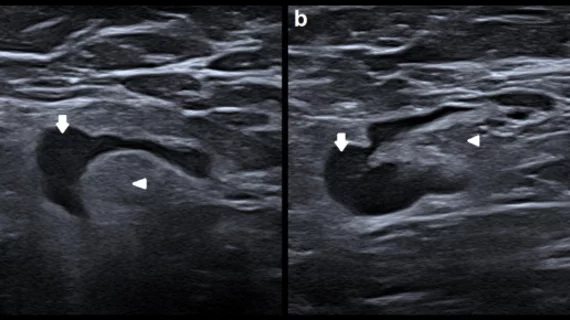
A new paper published in the European Journal of Radiology details how researchers utilized ultrasound images of benign reactive lymph nodes to retrain an earlier edition of an artificial intelligence model so that it would recognize vaccine-related lymphadenopathy. In doing so, they were able to produce a model that yielded 92.7% accuracy when differentiating between benign and malignant nodes. In comparison, radiologists’ visual inspection achieved an accuracy of 69.7%.
Researchers included 180 new, specially selected images from 154 different patients to build on the model’s prior performance. The images were divided into two groups—one to retrain the prior model and one to evaluate the improved model’s capabilities. Previously, the model had been tested for the use of diagnosing axillary lymph node involvement in breast cancer.
Adding to the positive finding of the model’s high accuracy when distinguishing between reactive and malignant nodes, experts also found that it achieved higher sensitivity and specificity when compared to radiologist assessments, at 71.8% vs 41.7% and 100% vs 83.6%.
“This direct comparison on the same images clearly suggests that the proposed methods can improve radiologists’ performance and also indicate that visual techniques are not enough to correctly classify nodes in patients after COVID-19 vaccination,” corresponding author David Coronado-Gutiérrez, of the Barcelona Center for Maternal-Fetal and Neonatal Medicine, and colleagues suggested. “These results demonstrate that these techniques have potential to detect unaffected lymph nodes even if they look visually similar to a metastatic one to the naked eye.”
The authors shared that although larger studies are needed to validate their findings, they do believe their model could play a vital role in non-invasively determining lymph node status when reactive adenopathy is in question. They indicated that the techniques could be integrated into software or ultrasound equipment for use in everyday clinical practice.
The detailed research can be viewed in the European Journal of Radiology.
More on vaccine-related lymphadenopathy:
Reactive lymphadenopathy slower to resolve after Moderna COVID vaccination
Experts suggest new follow-up imaging protocols for vaccine-related lymphadenopathy
These ultrasound features distinguish between COVID vaccine-related and malignant adenopathy
Reference:
David Coronado-Gutiérrez, Sergi Ganau, Xavier Bargalló, Belén Úbeda, Marta Porta, Esther Sanfeliu, Xavier P. Burgos-Artizzu. Quantitative ultrasound image analysis of axillary lymph nodes to differentiate malignancy from reactive benign changes due to COVID-19 vaccination. European Journal of Radiology, 2022.