Q&A: New Zealand father, son scientists discuss development of 3D color x-ray scanner
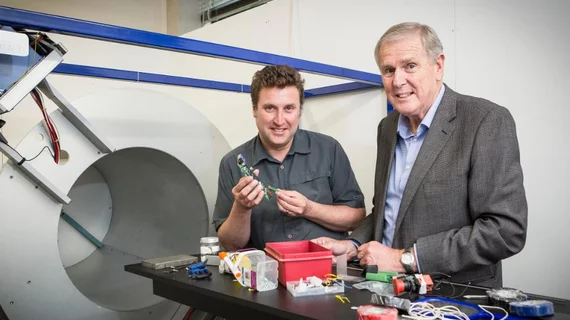
Last week, father-and-son scientists Phil Butler, PhD, a professor of physics and adjunct professor at the Human Interface Technology (HIT) lab at the University of Canterbury in New Zealand, and Anthony Butler, PhD, head of the University of Otago's radiology department and researcher at the University of Canterbury in New Zealand, imaged their first human subject with the MARS spectral x-ray scanner, a new 3D color x-ray machine.
The scanner project began in 2006 and has since grown to include a team of 40 researchers from both of their respected universities, dozens of international collaborators, and has garnered continuous support from the European Organization for Nuclear Research (CERN) and the New Zealand government. Their company MARS Bioimaging Ltd. currently sells small bore spectral CT scanners for pre-clinical medical research.
Health Imaging recently spoke with Phil and Anthony Butler about their MARS scanner, which has produced images more detailed than MR or CT. technology.
Health Imaging: Is this an enhanced CT machine or an x-ray machine?
Phil Butler, PhD: It is a CT machine, and it's using x-rays. One of the hopes for the future is that you will only need one scan — you'll need a MARS scan or a spectral CT scan. Our camera is different than a standard CT. Our pixels are roughly 10 times smaller. Since it's a volume effect, we've got a thousand voxels a thousand times smaller, so we can see much smaller things.
Does the MARS scanner have the same hardware as an x-ray or CT machine?
Anthony Butler, PhD: It uses standard x-ray, so we use a completely normal, off-the-shelf x-ray tube. The x-ray detector we use is called Medipix3 and was developed by more than 20 universities worldwide and a collaboration hosted by CERN (the European Organization for Nuclear Research). It basically takes the same photon-counting technology that CERN developed and puts that into a multi-energy detector, so we can measure up to eight energies at once, and we can do it at a pixel size of about 110 microns. We do it with an energy resolution of two to three kV depending on how the detector's set up. So, it's taking dual energy systems to the next level.
Phil Butler: We use the same x-ray tube for a standard CT, but it's actually a much lower-powered tube, and the acquisition time is much longer. We have an x-ray camera that measures the spectrum of the x-rays. CT systems are all black and white; they only measure the grayscale. There are a small number of systems on the market now that will use two colors, but we use a range across the spectrum.
What information is the MARS scanner using to determine color in the images produced?
Phil Butler: We use the color of the x-rays, and some people don't like calling x-rays “color,” because it's like infrared light or ultraviolet light. But many people are very happy to say these different energies from across the spectrum are effectively different colors. We use that extra information to decide and measure what atoms are in the sample we studied and because we've got that extra information, we can tell what atoms they are—whether they're calcium atoms or iodine atoms. We then get an image of water or tissue image of the object. We color those separately and put those together, and the images are the materials being colored.
Anthony Butler: What we're measuring is the atomic composition. We then use that information to use modified CT algorithms to identify and quantify materials. Basic quantitative information is available with x-rays, but it's been very, very hard for people to measure it in the clinical setting. If you've only got a standard x-ray film or a standard CT, you just can't measure that. You just ignore it. But by measuring quantitative data with encyclic electronic supply modern algorithms, you can start to do that technique not in a specimen in a lab but in a clinic.
What is the sensitivity of your scanner? What health risks could it pose to patients?
Anthony Butler: We've been looking at the carotid arteries, and we've been studying them for almost 10 years with our smaller scanners. We know we can see fat and water and then can start to see the micro calcifications. We're getting a hint that we can see the microhemorrhages within atheromas. How that translates without looking inside living people and how that then translates to management will be the focus of the next few years. So, we're really at the start of a journey.
Phil Butler: Because we are more sensitive in detection, we will need less contrast agents, so we get a lower x-ray dose, which is not particularly important unless you’re pregnant or very young. But a lower contrast agent is much more important if you're elderly. The promise is to be safer. For x-ray doses, there is a risk, but that risk is always less. The information you find is always so much more important than the risk.
How do you think the MARS scanner will change the cost of imaging exams when the technology will be implemented into hospitals?
Anthony Butler: I think it's a little bit like the introduction of any modality. Does an MRI reduce the cost of patient care? Yes, because we've learned more about the patient. We've learned better ways to manage them. But another view is you actually start treating the patient and costs go up, so the economics is a complex problem. In general, if you can measure disease better, then you can make more accurate diagnoses and that usually reduces costs and produces better patient outcome. If you can follow the treatment, you are providing the right therapy.
What sets the MARS scanner apart from other imaging modalities?
Anthony Butler: My gut feeling is that the energy information, being able to measure tissues, is really what's going to set it apart. CT is very fast; it's very high resolution. There's only a few applications where going fast will be helpful, but having more information will be broadly helpful across many more diseases.
Phil Butler: It's two factors—the first is the spectral or color factor, usually the spectrum or color of the x-rays. The second thing that distinguishes it from other clinical machines is our much smaller pixel size or voxel size.
What originally motivated you both to develop the scanner?
Anthony Butler: Excitement. One of my career goals is to have an impact on medical imaging because I find it fun. But also, it's also very rewarding knowing that you can have such an impact.
Phil Butler: I've pretty much always been within the university system, and this came up near the end of my career. I thought it was interesting, it was challenging, it was a fun problem—but once I got into it, I said this [scanner] is going to be helpful to people.