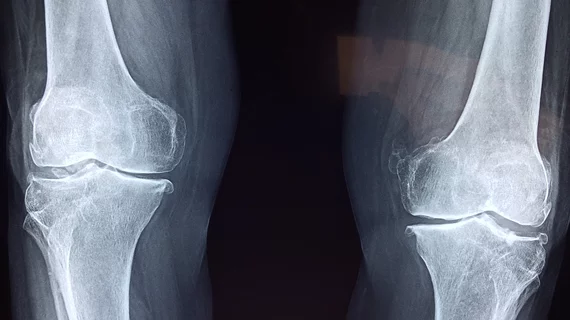
Minimally invasive interventional radiology procedure delivers relief to OA patients
A minimally invasive, intra-arterial procedure completed by interventional radiologists is gaining popularity among physicians and patients.
Geniculate/genicular arterial embolization (GAE) was originally developed for use in patients with knee hemarthrosis, but in recent years the procedure has become more widely utilized by interventional radiologists for the treatment of mild-to-moderate knee osteoarthritis (OA), a painful condition that can drastically deteriorate patients’ quality of life.
“Other therapies, including medicines and steroid injections, seek to mask the symptoms of osteoarthritis to provide relief,” David Prologo, MD, associate professor at the Emory University School of Medicine in Atlanta, said in a news update issued by RSNA on Tuesday.
Prologo, who has been performing GAE procedures for more than five years, continued, “Not only do those other options not affect the progression and pathology of OA, but they also carry significant risks of side effects.”
During the procedure, the IR embolizes geniculate branches that are responsible for pain in specific areas of the knee, which are identified before the procedure using palpitation and angiography. This reduces inflammation, cartilage degradation and the sensory nerve growth of OA.
A study published recently in the Journal of Bone & Joint Surgery found that 68% of patients who underwent a GAE procedure experienced significant reductions in pain and improved overall function. These effects lasted for more than a year, according to Sid Padia, MD, author of the study and director of interventional radiology at UCLA Medical Center in Santa Monica, California.
“There is a general unmet need for people with symptomatic knee OA for whom conservative treatments such as joint injections and physical therapy have not been effective, and who are not interested in pursuing total knee arthroplasty,” explained Padia, who has been performing GAE procedures since 2018. “GAE has the potential to fill this treatment gap.”
The minimally invasive outpatient procedure can be completed in around 1-2 hours. It is currently still considered to be a treatment in development and is therefore offered only at select centers in the U.S., but clinicians who currently perform the procedure are hopeful that it will soon become more widely available as larger clinical trials are completed.
More orthopedic imaging content:
AI tool achieves excellent agreement for knee OA severity classification
Multi-slice knee MRI technique saves time without sacrificing quality
New guidance for knee cartilage MRI seeks to prevent irreversible osteoarthritis
Routine CT scans offer radiologists opportunity to detect costly bone problems