Algorithm spots enteric tube misplacement on x-ray with great accuracy
Experts recently trained and validated an algorithm that can identify enteric tube misplacement on chest radiographs with great accuracy.
The deep learning algorithm was able to spot these harmful misplacements with 92% accuracy after being trained on nearly 5,000 radiographs and externally validated using more than 1,500 radiographs with real-world incidence of critically misplaced tubes. Clinical Imaging has published the study's results.
“Confirmation of correct enteric tube position within the stomach before use is essential. Introduction of fluids via an enteric tube into the airways can have dire consequences, ranging from aspiration pneumonia, respiratory failure and death,” corresponding author D.H. Mallon, from Imperial College Healthcare NHS Trust in London, and colleagues explained.
The researchers shared the most recent Never Event Report from NHS England indicated that up to half of enteric tube misplacements were due to radiograph misinterpretations. This highlights a concern for patient safety, as well as the need for a more automated method of confirming tube placement, they suggested.
That need is what led the researchers to develop and test a model based on a convolutional network that can accurately determine whether enteric tubes are critically misplaced within the respiratory tract.
On the external test set, 4.4% of tube misplacements were considered critical. The model was able to identify those misplacements with 92% accuracy, 80% sensitivity and 92% specificity. Of note, these numbers were in line with the internal validation figures, without any significant variations or dips.
“As there was no significant drop-off in model performance on the external test set, this suggests that the model generalizes well to independent data,” the authors wrote. “The model's generalizability is likely to have been aided by the multiple pre-processing and data augmentation steps, such as contrast equalization and re-alignment, which reduces the effect of technical variation caused by differences in the radiograph acquisition using different hardware.”
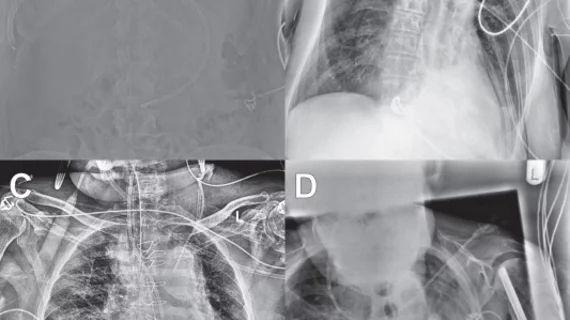
There were instances of false positives when sharp edges, such as ECG leads, within the lower zones were present, and also with false negatives when more than one tube was visualized in the radiograph—both problems that could potentially be avoided with segmentation of the enteric tube prior to classification, the experts shared.
The researchers concluded that although the model was able to quickly and accurately identify tube misplacement, the instances of false negatives prevent it from being able to operate independently just yet, as it would still require radiologist review.