Radiologists' understanding of tumor 'mimics' vital when assessing bone and soft tissue lesions
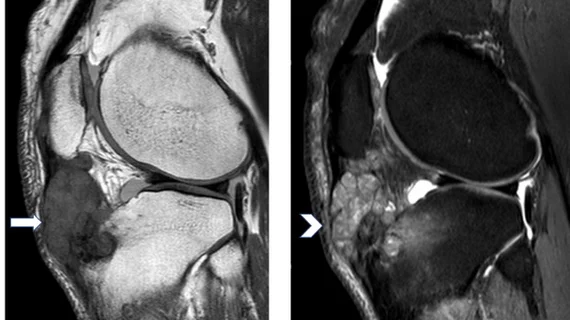
Many pathologies can mimic neoplastic bone and soft tissue tumors and deciphering the origins—whether malignant or benign in nature—accounts for a sizable portion of radiology referrals.
A new paper published in the European Journal of Radiology recently conducted an overview of the instances of non-neoplastic findings in bone and soft tissue lesions that had been referred to a multidisciplinary team (MDT) within the Oxford Bone and Soft Tissue Tumor Service to rule out malignancy. In 2020, the team received 976 referrals for patients with suspected sarcoma, of which 8.6% (84/976) received a biopsy-proven outcome of non-neoplastic pathology.
The authors of the study explained that, although most of these tumors present in a similar way—with a lump or localized pain—their origins are wide-ranging and require the use of additional imaging to characterize the lesion.
“BST can be benign or malignant and encompass bone sarcomas and soft tissue sarcomas. As neoplasia of mesenchymal origin, they can arise in bone, cartilage, fat, vascular and hematopoietic tissues,” corresponding author Faheem Ahmed Malik, of Oxford University Hospitals NHS Foundation Trust, and co-authors wrote. “Consequently, they comprise a broad number of distinct histopathological malignancies, with over 160 different subtypes listed in the most recent World Health Organization (WHO) classification.”
The 8.6% of non-neoplastic findings were comprised of a broad range of tumor-mimicking pathologies. The authors categorized them as follows:
Vascular: 32.1%
Inflammatory: 31%
Traumatic: 14.3%
Degenerative: 6.0%
Idiopathic: 6.0%
Infective: 4.8%
Metabolic: 3.6%
Autoimmune: 1.2%
Genetic: 1.2%
The authors acknowledged that while 8.6% of 976 referrals may seem like a low rate of benign cases, most non-neoplastic pathologies are caught before being sent for review by a multi-disciplinary team. Radiologist review is crucial in limiting these referrals to only the most serious cases—their understanding of how sarcoma mimics can present on imaging could potentially prevent patients from having to undergo invasive procedures to rule out malignancy.
However, in these instances of highly suspicious imaging presentations, the authors allude to a “better safe than sorry” mentality.
“We suggest that clinicians should continue to maintain a high index of suspicion in aggressive-looking bone and soft tissue lesions, and that histopathological analysis should always be sought in cases of ambiguity.”
The study abstract can be viewed here.