Combined, alcohol dependence and depression cause 'severe and extensive' brain connectivity impairment
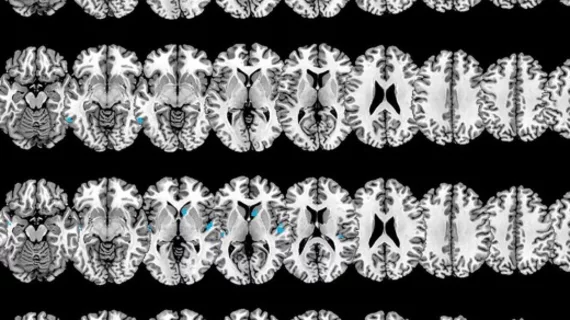
Alcohol dependence and depression can each affect the functional connectivity of the brain, but when the two co-occur, connectivity between certain regions is significantly worse, a new MRI study shows.
In a paper published in Academic Radiology, researchers highlight the effect of comorbid alcoholism and depression on areas of the brain related to emotional regulation, fatigue, stress, reward learning and motivation. Although decreased connectivity patterns in these areas were observed in both people with alcohol dependence alone and depression alone, those who struggled with both conditions simultaneously showed greater connectivity deterioration.
“The presence of alcohol dependence increases the risk of depressive disorders, and the presence of depressive symptoms also promotes the maintenance and recurrence of alcohol dependence and complicates the clinical presentation and course of alcohol dependence,” corresponding author Xiaojian Jia, with the department of addiction medicine at Shenzhen Clinical Research Center for Mental Disorders in China, and colleagues explained. “It has been reported that compared to patients with alcohol dependence alone, patients with alcohol-dependent comorbid depressive disorders had more severe clinical symptoms, a longer course of disease, a higher rate of relapse, and a worse prognosis and quality of life”
For the study, experts analyzed the resting state functional MR imaging of 29 alcohol-dependent patients with depression, 31 alcohol-dependent patients without depression and 31 healthy control subjects.
In alcohol dependent participants, imaging showed decreased connectivity between the left amygdala and the right caudate nucleus, and between the right amygdala and right caudate nucleus, right transverse temporal gyrus, right temporal pole, and superior temporal gyrus.
Significantly worse connectivity was observed in each of these regions in alcohol dependent patients with depression; however, functional connectivity between the right amygdala and the left middle temporal gyrus was also prevalent. This finding appears to get worse over time.
Many of these regions are within either the reward network (also known as the mesolimbic dopamine system) or the limbic system. The reward system is closely linked with the development of alcohol dependence, while impairment of the limbic system’s structure or function has been linked with depression. Something these areas both have in common is the amygdala.
“The amygdala is not only an important component of the reward network, but also a key brain region of the limbic system,” the experts wrote. “The amygdala has extensive connections with cortical and subcortical structures and plays an important role in human daily life by participating in many functions of the human brain, such as reward, emotion, motivation, memory and attention.”
Recent research has suggested that impaired amygdala function could be related to numerous psychiatric disorders, including both alcohol dependence and depression. The decreased connectivity observed in this study between the amygdala and nearby regions “may be the explanation to alcohol-dependent comorbid depression.”
“Besides providing a reference for exploring the comorbidity of alcohol dependence and depressive disorders, this study also provides a potential target for the intervention and treatment of comorbid patients.”