Does obesity improve lung cancer outcomes? Yes, to some extent
Although obesity is a known risk factor for developing serious health conditions, such as diabetes and cardiovascular disease, new research suggests that it may actually benefit patients with non-small cell lung cancer.
Authors of a new analysis in the journal Radiology indicate these new findings could help explain the “obesity paradox,” wherein being overweight is linked to both improved outcomes in certain diseases and increased mortality rates in others. Obesity's association with improved clinical outcomes could be owed to how body mass index is measured, they suggest.
“The inclusion of BMI as a primary measure of obesity is based on its simplicity, practicality, and widespread use in clinical settings. However, BMI does not differentiate between muscle and fat mass or provide information on fat distribution, such as subcutaneous and visceral fat, which are critical for understanding metabolic health and cancer prognosis,” Juhee Cho, with the Center for Clinical Epidemiology at Sungkyunkwan University, Samsung Medical Center in Seoul, South Korea, and colleagues explained. “Recent research has shifted toward a more nuanced understanding of body composition, recognizing the important role of skeletal muscles, particularly in patients with cancer.”
Simply put, having a BMI that falls in the obesity category does not necessarily mean that an individual is at greater risk of cardiometabolic-related conditions or side effects. But does a higher BMI have advantages with respect to cancer mortality?
Yes, but there are caveats, the authors explained.
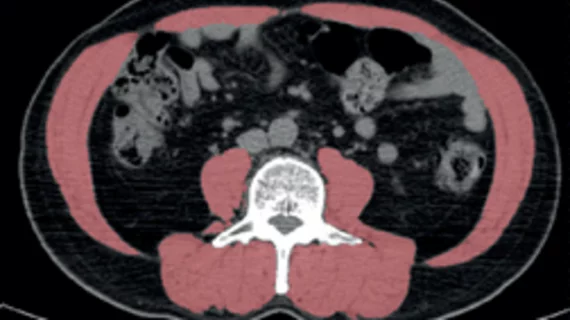
The retrospective study included over 7,000 patients with non–small cell lung cancer who underwent curative resection between January 2008 and December 2019. Patients were divided into two groups—obese and the opposite, according to basic BMI metrics—and had available CT scans for the team to analyze. Measurements of skeletal muscle at the level of the third lumbar vertebrae were taken and compared among both groups.
In the obese group, patients who were without both low skeletal muscle mass and the presence of myosteatosis had improved overall survival rates. However, these findings were only observed in male patients and among those who had a history of smoking, according to the data. The obese cohort had a 21% decreased risk of death compared to the other group.
“Based on the findings of this study, it is proposed that patients with obesity whose skeletal muscle quality and quantity are preserved may drive the obesity paradox, emphasizing the essential contribution of skeletal muscle to this phenomenon,” the authors noted. “Although BMI is a useful and practical tool for initial assessment, it should be complemented by detailed body composition measurements to better understand the obesity paradox in non–small cell lung cancer.”
Learn more about the findings here.