Factors that increase the likelihood of false results on prostate MRI
Certain clinical and imaging factors can influence the likelihood of patients receiving either false positive or false negative results based on prostate MRI.
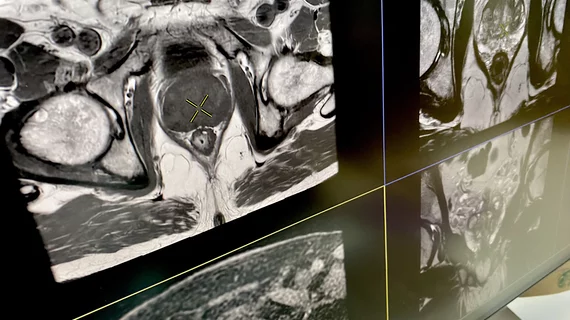
The utilization of multiparametric prostate MRI (mpMRI) has been growing in popularity in recent years, and multiple studies have indicated that mpMRI results could be used to diagnose cancer without the need for invasive biopsies. However, false positive and false negative results are common when using MRI alone, which has prompted concern over its reliability.
A new paper in Radiology dives into how different elements affect the accuracy of mpMRI using the Prostate Imaging and Reporting Data System version 2 (PI-RADS v2). Experts involved in the study are hopeful that their findings can improve the accuracy of diagnosing prostate cancer.
For their research, the team examined the cases of more than 2,500 patients who underwent mpMRI between October 2016 and July 2022. To be eligible, patients’ exams had to contain zero or one PI-RADS v2 category 3–5 lesion. Thirteen radiologists reviewed the exams, defining false negatives as having a PI-RADS score of 2 or lower but grade group 2 or higher prostate cancer at subsequent biopsy; false positives were defined as scores of 3 or higher but labeled as benign or grade group 1 cancer at biopsy. Readers were tasked with identifying common patterns that predicted false results.
Of the 2,548 patients included in the analysis, 52% had false positive results and 15.8% had false negative results based on imaging. False positive results were more common among younger patients with low PSA levels who also had smaller lesions and transition zone lesions. In contrast, false negatives were associated with two factors.
“PSA density and patient age independently predicted false positive and false negative results for detection of prostate cancer at mpMRI using PI-RADS v2,” Matthew S. Davenport, MD, with the Department of Radiology at Michigan Medicine, and colleagues noted. “These factors are not part of the PI-RADS v2 algorithm and may inform mpMRI interpretation to improve prostate cancer diagnosis.”
The group suggested the factors identified in their study should be considered when deciding whether to send patients for additional assessments to confirm or rule out malignancies.
Learn more about the findings in the study abstract, available here.