Algorithm reduces NSCLC tumor segmentation times by 65%
A newly developed deep learning algorithm has the potential to turn a historically time-intensive process into a task that takes mere seconds, saving valuable time for clinicians treating patients with non-small cell lung cancer.
The algorithm is said to accurately identify and segment tumors visualized on CT scans. A new analysis published in Lancet Digital Health showed that physicians who utilized the algorithm were able to precisely target tissue for radiation therapy planning at times up to 65% faster than traditional manual methods.
Corresponding author of the study Raymond Mak, MD, of the Brigham’s Department of Radiation Oncology, and colleagues explained how this new AI method is beneficial for both patients and clinicians:
“The benefits of this approach for patients include greater consistency in segmenting tumors and accelerated times to treatment. The clinician benefits include a reduction in mundane but difficult computer work, which can reduce burnout and increase the time they can spend with patients.”
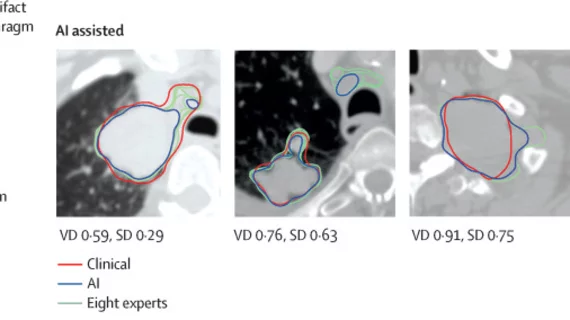
In a close collaboration with radiation oncologists, the experts trained their model on the CT lung images of 787 patients and tested on the scans of more than 1,300 patients from external datasets. To examine the segmentation performance of the algorithm, eight radiation oncologists were asked to complete manual segmentations on images and then perform blinded ratings of the segmentations performed by other physicians and the algorithm.
Researchers noted similar performances between the physicians and the algorithm when working alone. However, the radiation oncologists spent 65% less time editing the algorithm’s segmentations, which also resulted in 32% less variation in the edits. The AI segmentations were rated higher by the clinicians as well.
The authors noted that their validation approach could provide a steppingstone for reliably implementing AI into physicians’ clinical practice in the future. They are continuing their studies on the relationship between clinicians and AI to ensure that the evolving applications improve, rather than degrade, clinical care.
“This study presents a novel evaluation strategy for AI models that emphasizes the importance of human-AI collaboration,” said co-author Hugo Aerts, PhD, of the Artificial Intelligence in Medicine Program, Mass General Brigham, Harvard Medical School. “This is especially necessary because in silico (computer-modeled) evaluations can give different results than clinical evaluations. Our approach can help pave the way towards clinical deployment."
The detailed research can be viewed here.