Could synthetic images replace the need for contrast?
Deep learning techniques could eliminate the need for contrast during MRI scans used to screen for and stage prostate cancer.
According to new research published Tuesday in Radiology, it is possible to generate simulated contrast-enhanced prostate MRIs using a deep learning model trained to synthesize images from noncontrast sequences. What’s more, the resultant images are of diagnostic quality and can be reliably used to assess clinically significant prostate cancer while also sparing patients from contrast exposure, experts involved in the study suggest.
Contrast-enhanced sequences add great value for readers when the quality of T2-weighted imaging and DWI sequences is poor. However, there are caveats that accompany using gadolinium-based contrast agents (GBCAs), including the related costs and concerns regarding accumulation of the agent over time. Artificial intelligence could be the key to filling in the gap between accessibility and exam quality, authors of an editorial accompanying the new paper signal.
“Omitting intravenous contrast material may reduce scanning time, may be more cost effective and may allow more male patients access to MRI, an important consideration with the projected incidence of prostate cancer,” write co-authors Radhouene Neji, MD, and Vicky Goh, MD, both with the School of Biomedical Engineering and Imaging Sciences at Kings College London. “Amid ongoing debate and with results of prospective trials yet to be published, research into artificial intelligence to synthesize contrast-enhanced MRI scans is timely and relevant.”
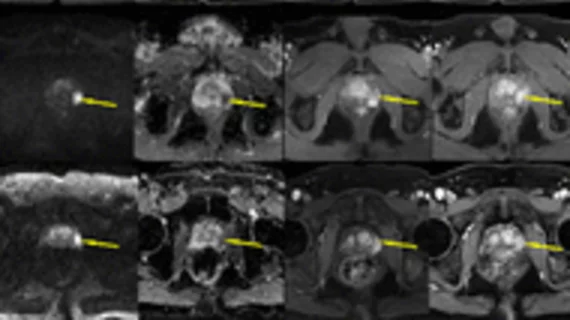
For the research, the team deployed the pix2pix generative AI model to create synthetic, T1-weighted, contrast-enhanced images using unenhanced sequences and apparent diffusion coefficient maps. The model was trained on a dataset of 244 patients from one institution and was tested on an additional three datasets (one internal, two external) of patients scanned on different MRI equipment at other institutions. Three readers blinded to image type interpreted the scans.
Both the simulated and actual contrast-enhanced images showed high similarity and achieved excellent reader agreement of PI-RADS scores. When simulated images were included in biparametric MRI reads, nearly 11% of patients had their PI-RADS scores changed from 4 to 3.
The authors suggest their findings indicate simulated contrast-enhanced MR images could pose as a suitable alternative when trying to avoid GBCA use, though more research is needed before this method achieves clinical utility.
The study abstract is available here.