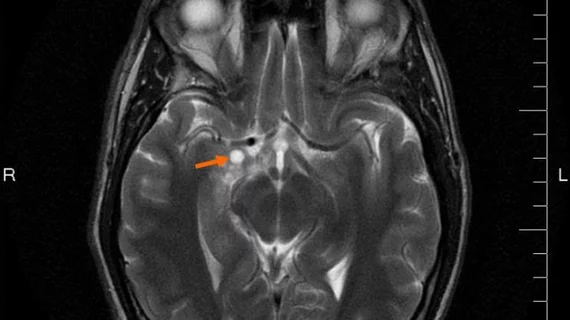
Deep learning–MRI classification combo called a ‘great leap forward’ in glioma care
Using brain MRI and a deep learning network, researchers have achieved 97% accuracy at classifying a gene mutation indicative of growth in localized gliomas.
If the science translates to the clinic, it may save many patients from having to undergo brain surgery for tumor biopsy.
A study describing the research, conducted at UT Southwestern Medical Center in Dallas, is running in the spring edition of Neuro-Oncology.
The gene at the heart of the investigation, isocitrate dehydrogenase (IDH), has emerged as an important prognostic marker in gliomas, according to the study abstract.
In the study, the image data and corresponding genomic information used to train the algorithm came from 214 patients whose deidentified data are stored in the Cancer Imaging Archive and the Cancer Genome Atlas, both of which are funded by the National Cancer Institute.
Part of the breakthrough was the research team’s use of a single algorithm to gauge the mutation status. Previous techniques have needed hand-drawn supplements or additional AI models to identify tumor boundaries or detect potential mutations, according to UT Southwestern’s own coverage of the advance.
In the coverage, senior study author Joseph Maldjian, MD, calls the ability to determine the status of a particular mutation status in gliomas using only conventional imaging and AI “a great leap forward.”
Eventually the advance may lead to nonsurgical tumor resection, he suggests, meaning patients wouldn’t have to go under the knife for either prognosis or treatment of brain tumors.
By omitting the need for image preprocessing and using images routinely acquired from glioma patients, Maldjian says, the team has created “an ideal scenario for easily transitioning this [research] into clinical care by using images that are routinely acquired.”
Meanwhile prior efforts to get to this point in similar fashion never topped 90% accuracy.
“In the big picture, we may be able to treat some gliomas without operating on a patient,” says Maldjian, who is chief of neuroradiology at UT Southwestern’s O’Donnell Brain Institute. “We would use AI to detect an IDH-mutated glioma, then use IDH inhibitors to slow down or reverse the tumor growth.”
The field of radiogenomics, he adds, is “exploding with possibilities.”