Does display color scale affect diagnostic imaging performance?
The color scale used to optimize image interpretation has a measurable diagnostic effect on the interpretation of computed tomography perfusion (CTP) exams and apparent diffusion coefficient (ADC) images, according to an Oct. 15 study published in Clinical Radiology.
“Color-coded maps are the preferred visualization approach in most recently developed imaging techniques; however, no standards or guidelines are available for radiologists to use in deciding on a color scale that optimizes image interpretation,” wrote first author Silvina Zabala-Travers, MD, with Diagnostics and Software Reliability’s Division of Imaging, part of the FDA, and colleagues.
The team set out to determine whether the choice of color scale affects malignant prostate tumor detection and characterization in ADC maps and myocardial ischemic lesion detection and transmural extension assessment in CTP.
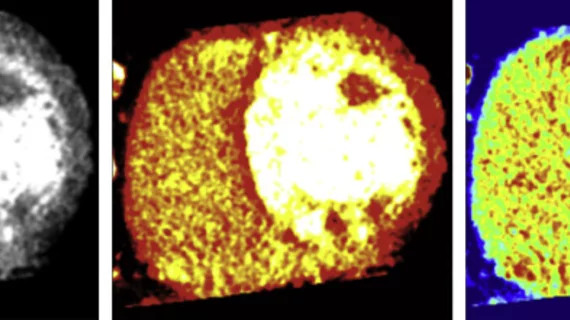
Twelve clinicians with varying levels of experience read 210 myocardial CTP exams while nine interpreted 165 MRI ADC prostate images. Broken into three separate reading sessions, each reader scored their confidence for tumor detection and ischemia on a scale from zero to 100. Each analyzed the same scan using grayscale, hot-iron and rainbow scales.
According to the results, for lesion detection on CTP the area under the receiver operating characteristic curve (AUC) was up to .10 higher (.67±0.02) with greyscale, compared to rainbow (.56±0.02); Detection with hot-iron was between .61±0.03. For ischemic transmural lesion categorization, inter-reader agreement was highest with grayscale.
For prostate tumor detection, there was a “small tendency” for rainbow and grayscale to beat out hot-iron, the authors wrote.
“The present findings indicated a measurable effect of color on image interpretation that merits further investigation, with study designs focusing on reducing variability in order to provide optimal presentation in imaging techniques relying on color visualization,” they concluded.