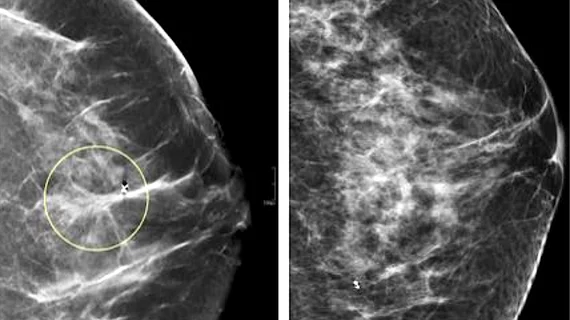
Standalone AI excels at reading digital mammograms, but how does it hold up with DBT exams?
The ability to use artificial intelligence as a standalone reader in medical imaging could be on the cusp of becoming reality, according to a new meta-analysis published this week in Radiology.
The paper summarizes 16 different studies on AI as a standalone reader for digital mammograms and digital breast tomosynthesis (DBT) exams, published between January 2017 and June 2022. This included a total of more than 1 million exams of nearly 500,000 women.
“There is considerable interest in the potential use of artificial intelligence systems in mammographic screening,” co-senior author of the new paper Linda Moy, MD, with the New York University Grossman School of Medicine, and colleagues noted. “However, it is essential to critically evaluate the performance of AI before it can become a modality used for independent mammographic interpretation.”
The team’s own evaluation included six reader studies, seven historic cohort studies on digital mammography, and four studies on DBT. In the DM studies, standalone AI systems achieved significantly higher pooled AUCs in comparison to expert readers but performed slightly inferior in the historic cohort studies. AI also recorded higher AUCs in the DBT studies, though the authors noted that there was not enough data to sufficiently assess standalone AI’s utility in DBT screenings.
In an editorial accompanying the study’s results, Anabel Scaranelo, MD, assistant professor in the breast imaging section of the Department of Medical Imaging at the University of Toronto, notes that AI in breast cancer screening settings can address a number of shortcomings in the field of radiology, but that the field is not ready to let such technology freely fly just yet.
“In breast imaging, greater than 99% of the more than 20 million mammographic screenings performed in the United States each year are normal,” Scaranelo noted. “Hence, having a standalone AI unit that can independently read and sign out those normal cases could significantly reduce radiologist fatigue, as AI is diligent and never tires of repetitive tasks.”
However, Scaranelo pointed to several hurdles that remain between standalone AI and clinical practice, including limitations in access to data and a slew of medicolegal issues. So, while the meta-analysis findings show potential, rigorous prospective testing is still needed, Scaranelo and the authors of the meta-analysis noted.
The study abstract is available here, and the editorial here.