Eye-tracking study shows radiology reporting via voice commands becoming more viable
Researchers used eye-tracking to measure if the “positive findings only” radiology reporting style could improve the accuracy and generally hold the attention of radiologists. The reporting style utilizes voice commands to map positive findings to radiology reports — and a study from Florida International University shows it works when supported by technology, reducing dictation time and improving the focus of radiologists. The results are published in the European Journal of Radiology. [1]
AI that understands speech and converts it into text has been on the market for years. However, the technology is still somewhat unreliable, suffering from problems with accuracy. This puts more burden on radiologists who, after utilizing voice commands to make report findings, were forced to make edits. This led to errors in reporting, the authors of the study noted, and ultimately increased turnaround time.
For now, voice dictation utilizing commands is mostly used with a positive findings-only reporting style — which itself is not all that commonly used, according to the research team led by Mona Roshan, an MD candidate at Florida International University. She and her colleagues aimed to figure out if the reporting style would become more viable and common if the technology improved.
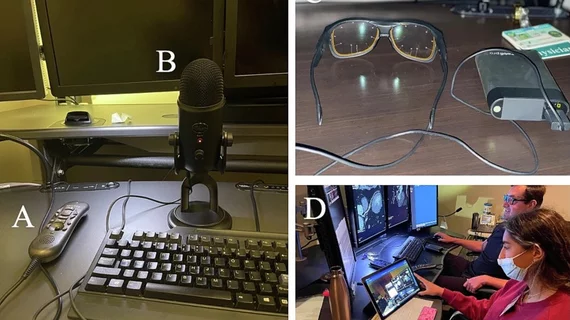
To conduct the study, two board-certified radiologists reviewed chest X-rays, CT scans, and MRI images. Researchers monitored as the radiologists made reports, using a standalone microphone in 76 cases for voice command-based, positive findings-only reports. To compare, 81 cases were reported using a standard dictation.
Eye-tracking was deployed in both cases, with digital eyeglasses used to measure data on dictation time, interpretation time, and ultimately the time it took to fully examine and make a report. The eye movement of the radiologists was measured using recordings from the eyeglasses to monitor the effectiveness of utilizing voice dictation for both reporting styles, and to better understand what radiologists focus on when producing reports.
“From the recordings of the eye tracker device, thermal heat maps were generated for each style. As a graphical representation of the data, the thermal heat map visualizes the areas on the monitors in which the radiologists viewed the most (red) to least (green) throughout their case reviews,” the authors wrote. “By comparing the thermal heat maps of both styles, the differences in the locations at which the radiologist looks at the most and least can be demonstrated. Reading sessions were performed on different days to capture different modalities and settings, such as outpatient, inpatient, and emergency department radiology workflows.”
The researchers found that positive findings-only reporting, utilizing both voice commands, not only reduced reading time but also improved the focus radiologists had on medical images, as judged by the heat mapping.
Specifically, the findings showed a substantial reduction in average dictation time to 16.54 seconds with the new dictation style, in contrast to the 29.39 seconds required for the standard style (p = 0.0003). Importantly, this efficiency gain was achieved without causing any significant impact on interpretation time or the overall examination duration. The interpretation time remained at 70.9 seconds, and the total examination time was 87.45 seconds for the new style, compared to 64.3 seconds (p = 0.78) and 93.69 seconds (p = 0.38) for the standard style, respectively.
“Our data confirms that implementing the positive findings-only dictation style using a standard structured reporting template and a stand-alone microphone can improve radiologists' performance by significantly enhancing accuracy and decreasing dictation time without compromising the interpretation and total examination times,” the authors wrote.
Ultimately, Roshan and her research team believe the study shows that a good quality microphone, along with advances in AI, may make voice-dictated positive findings only reporting a more viable option that clinical settings should consider adopting.