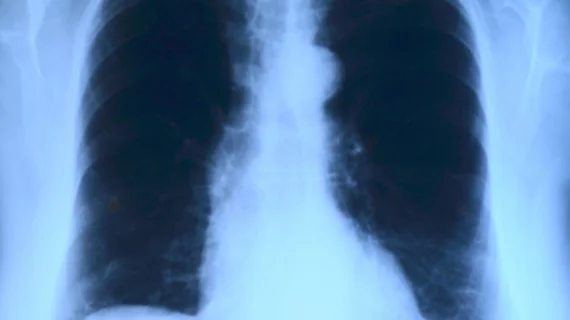
Chest x-ray used to analyze first US patient with coronavirus
The first U.S. patient with lab-confirmed coronavirus was diagnosed, in part, via chest radiography, according to a recently published case study. A growing body of evidence, however, suggests computed tomography is far more accurate at spotting abnormalities associated with this new virus.
In this case of a 35-year-old man in Snohomish County, Washington, with a travel history in Wuhan and four-day cough and fever, chest x-rays did not reveal lung abnormalities until his fifth night in the hospital and ninth day of sickness overall. Earlier studies, including one published Feb. 22, found that CT detects signs of COVID-19 even before symptoms appear.
And a more recent case, published in the Korean Journal of Radiology, determined that chest radiographs may even miss signs of the virus that are detectable when using CT.
For this initial U.S. case, published March 5 in the New England Journal of Medicine, the man’s first chest radiograph showed no abnormalities; lab tests, nose swabs and other clinical findings were also normal. Due to his travel history, clinicians at the Washington urgent care clinic and those at the state's Department of Health immediately called the Centers for Disease Control and Prevention to collect samples from the patient.
His real-time reverse-transcriptase–polymerase-chain-reaction (rRT-PCR) test came back positive for 2019-nCoV and he was taken to an airborne-isolation unit at Providence Regional Medical Center for observation. The location of this area limited the man to point-of-care lab testing at first, the authors noted.
During Day 3 in the hospital, another chest x-ray appeared normal, showing “no evidence of infiltrates or abnormalities,” first author Michelle L. Holshue, with the CDC’s Epidemic Intelligence Service, and colleagues wrote. But on Day 5 of hospitalization, a second x-ray showed evidence of pneumonia in the lower lobe of the left lung. This occurred as the man’s respiratory status changed.
The next x-ray exam—performed on Day 6 of the patient’s hospitalization—yielded abnormal findings, including “basilar streaky opacities” in each lung, consistent with atypical pneumonia, the group wrote.
On Day 8 of the man’s hospitalization, his clinical condition improved. And as of Jan. 20, he was still in the hospital with no symptoms except a cough, which was improving.
“This report highlights the need to determine the full spectrum and natural history of clinical disease, pathogenesis, and duration of viral shedding associated with 2019-nCoV infection to inform clinical management and public health decision making,” the authors concluded.
Read more about the case here and more of Health Imaging’s coverage of coronavirus here.