Q&A: Should COVID vaccinated patients delay getting breast imaging — new study says no
In the weeks after the first COVID-19 vaccines were introduced in early 2021, it was quickly discovered the COVID vaccine can cause swollen lymph nodes that could mimic cancer on mammograms. To avoid needless biopsies of this vaccine-caused axillary adenopathy, women were told to hold off several weeks before getting breast imaging after they were vaccinated. However, a new study recently published in Radiological Society of North America (RSNA) journal Radiology now suggests that women might want to consider going through a screening regardless of when they were vaccinated.
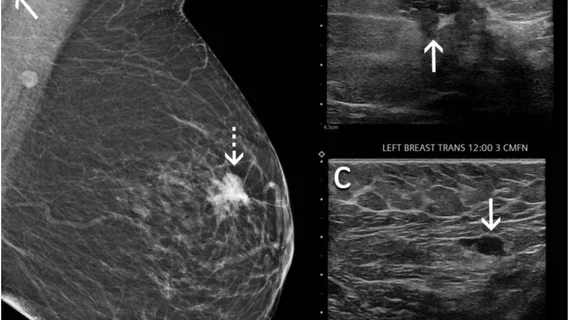
In the study, "Axillary Adenopathy after COVID-19 Vaccine: No Reason to Delay Screening Mammogram," published online Feb. 8, 2022, researchers conducted a retrospective analysis of patients who received their vaccination and had breast imaging in the first few months of 2021. The study included more than 1,200 individuals imaged across 17 New York University (NYU) sites. Of those, about 44% (or 537 patients) experienced lymphadenopathy on at least one exam. Providers identified swelling on mammography alone in 9% of cases, ultrasound alone in 61% and on both modalities at a 30% rate.
O the 8% of patients who underwent a biopsy, 79% were benign, while 21% had malignant results. Four patients were diagnosed with metastatic breast cancer and four patients were diagnosed with lymphoma. One patient with a known history of lung cancer was diagnosed with lung cancer metastatic to an axillary lymph node.
For this reason, the authors said delaying breast imaging in the COVID vaccination era should be reconsidered.
The lead authors of the study were Stacey Wolfson, MD, chief resident, and Beatriu Reig, MD, MPH, clinical assistant professor of radiology, both from the Department of Radiology, NYU Grossman School of Medicine. Below they share additional details from the study and its key takeaway.
Can you give an overview of the study?
Stacy Wolfson: Prior recommendations included delaying mammograms for about 4-6 weeks after receiving the COVID-19 vaccine. So our study is now the largest, most comprehensive dataset evaluating the effects of these vaccines and what we see on breast imaging thereafter. What we are seeing is a lot of patients are having this lymphadenopathy, or the swollen lymph nodes, on the same side of of the body where they received the vaccine. W were able to kind of track that and see how many people have had it and what the time to resolution is.
There were 1,200 patients in this study who had breast imaging and had also received the COVID vaccine during the study timeframe.
What we saw from our study is that it's very common — about 44% of the women that had breast imaging during this time period after receiving the vaccine had lymphadenopathy. And the time to actual resolution of this lymphadenopathy is pretty variable, with some patients having an extended period of time to resolution, including some patients experiencing this lymphadenopathy as long as 43 weeks after the vaccine. And because of that and our extensive information that we've gathered, we're seeing that this time to resolution is variable and it is common to have these swollen lymph nodes. So we are saying that maybe it's not recommended to actually wait during this time prior to getting your breast imaging after getting the vaccine.
What does the study mean? Should breast imaging centers just tell all patients to come in and the radiologists will know there will likely be swelling of the lymph nodes near where they got vaccinated, and they will just take it into consideration when reading the exam?
Stacy Wolfson: So I think it's important to always take into consideration the patient context and the patient's individual risk factors. I think it's important to state to patients that we do know this benign reactive lymphadenopathy is very common. A lot of patients are experiencing it and the time to actual resolution is extended and is variable. So it's important to have that in the back of your mind when you're seeing this in a breast image, or even as a patient is experiencing this. But, it's also important to realize that some people don't fit this exact kind of criteria [with vaccine-caused adenopathy] and they might have elevated risk factors─ current history or prior history of cancer. That changes how we need to evaluate their imaging and their story.
But this should be used as a basis for the general population, because it is common to have this lymphadenopathy after COVID vaccinations, and the time to resolution is kind of variable. It's not necessary to wait after receiving the vaccine to just have your general screening. Because it is common, depending on your risk factors and what the clinician would see, that further imaging is not necessarily warranted. The time to resolution is variable and you might be following up on a benign lymph node for multiple follow up time periods waiting for this resolution. But we don't actually know when it would truly resolve.
Should clinicians reassure patients that these findings are generally not a cause for concern with the lymph nodes and encourage them to come in?
Stacy Wolfson: I think it is important for clinicians to understand this and be able to also advise their patients that this is something that could happen after the vaccine.
Beatriu Reig: If you mean clinicians or patients who are noting palpable lumps in their axilla or pain in their axilla, we've seen that very commonly in our study on screening mammograms. But a certain small percentage of patients, 5% in the lymphadenopathy group, actually presented with palpable lumps. So it's not uncommon, and I think probably a lot of clinicians out there have already been experiencing this and reassuring their patients and following their patients. But of course we always say if there's ever a palpable lump or a focal pain or an area that is not explained by the clinical scenario or if it persists beyond the timeframe that the clinician might expect, have them come in and get their breast imaging. We're always happy to evaluate patients, screen them ourselves and figure out what's going on.
Previous research suggested delaying imaging for a few months and there was fear of going to doctors' offices because of COVID, so there were a lot of women who probably missed one or possibly two annual screenings. Are there fears of seeing increased levels of breast cancer, or finding more advanced breast cancers?
Beatriu Reig: That's a great question and a big fear in the breast imaging community. And certainly we've already seen those data come out. There was an article in Radiology last October showing that the numbers of breast cancers diagnosed in the early COVID pandemic period were much lower than in a similar time period six months before. Unfortunately, there are a lot of disparities also─ racial and socioeconomic disparities in the number of cancers diagnosed over the COVID pandemic, which will exacerbate breast cancer levels and in groups of women.
So we definitely expect to see more advanced cancers and worse outcomes down the line. Of course, that research is still ongoing, and just to stress that the initial recommendations of delaying 4-6 weeks after your vaccine have no comparison to the bigger effects of the COVID. The pandemic caused some women to miss a year, maybe even two years of screening, which is a harm that we are still seeing the effects of.
Now that we are living in this era of the new normal under COVID, do you think that the recommendation moving forward might be to just see everybody at their regularly scheduled appointments, regardless of when they received the vaccine or boosters?
Stacy Wolfson: I do think that could be a possibility of the new normal moving forward─ just accepting that non-reactive lymphadenopathy could occur after the vaccine and kind of having that in the back of our minds when we're reading these images. And I do think it's important, now that it's the new normal, to document when patients did receive the vaccine and which vaccines they had, just so that we could be fully informed as we're reading their scans.
Beatriu Reig: It is important not to delay mammograms.
Read more about this study in the article Mammograms should not be delayed after COVID vaccine, research shows.
Related COVID-19 Vaccine Imaging Content:
VIDEO: Should women wait to get mammograms after COVID vaccination?
Women do not need to delay their mammogram appointment after COVID-19 vaccination.
Molecular imaging group shares updates for managing COVID-19 vaccine effects on PET/CT exams
How radiology providers can minimize mammography recalls among COVID-vaccinated patients
Radiologists report COVID vaccine side effects mimicking breast cancer on mammograms
These ultrasound features distinguish between COVID vaccine-related and malignant adenopathy