Chest X-ray guidelines disappoint in the ED
Guidelines intended to reduce chest X-ray overutilization in emergency departments are not as effective as many had hoped, according to new data published in Cureus.
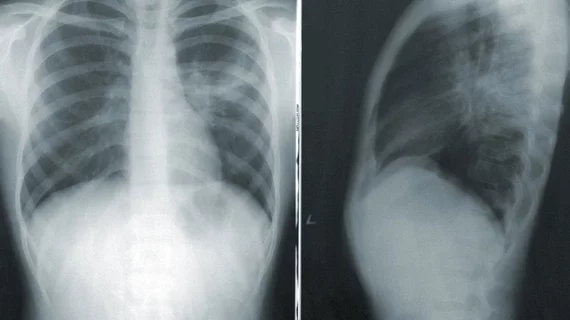
Chest radiographs are commonly requested upon the admission of new patients triaged through the emergency department. Corresponding author of the new Cureus paper Mark Richman, of the Emergency Department at Northwell Health Long Island Jewish Medical Center, and colleagues explained that not only does the baseline imaging often provide no added clinical value, but it can also be detrimental for provider organizations as well as patients [1].
“Adverse consequences of such CXRs include unnecessary radiation exposure, cost, time, and false positives, which can trigger a diagnostic cascade,” the authors explained. “Extraneous CXRs performed on already-admitted ED patients can delay inpatient transfer, thereby increasing boarding and crowding, which in turn may affect mortality and satisfaction.”
In 2016, internal medicine hospitalist services at Long Island Jewish Medical Center implemented guidelines concordant with those of the American College of Radiology to reduce the use of unnecessary chest imaging in the emergency department. After all ordering providers were educated on what did and did not warrant a chest x-ray in the ED, pre- and post-implementation data were assessed.
Through this the experts observed little to no changes in CXR requisitions among admitted patients with diagnoses that did not merit the imaging, but there was a slight decrease in orders for pre-admitted patients. However, the authors shared that this decrease could be attributed to patients with chief complaints that did not warrant chest imaging.
Cardiovascular disease, renal disease, hyperkalemia and being older in age were all associated with increased likelihood of patients undergoing chest imaging.
The researchers shared that these results were not expected, which prompted them to dig a bit deeper into the question at hand and ask hospitalists directly: “Why do providers on the internal medicine admitting service request an admission CXR for some admissions, even in the absence of non-cardiac/non-pulmonary concern?”
The answers were varied, but a few common themes among them included legal considerations, concerns for pulmonary edema when patients are given large amounts of fluid and a “desire to be comprehensive” when treating inpatients who could have additional subclinical diseases.
To learn more about the study, click here.