Routine CT scans offer opportunistic assessments of the parathyroid gland
Assessing incidental parathyroid findings visible on routine CT scans could lead to earlier diagnosis of primary hyperparathyroidism (PHPT) years before patients become symptomatic.
Such opportunistic assessments could “decrease existing diagnosis gaps,” according to a new study published in Academic Radiology.
“Fewer than 25% of patients with classic PHPT are referred for surgical evaluation. Not only is there substantial room for improvement in the diagnosis and treatment of PHPT, untreated PHPT conveys increased risk of heart attack, stroke, and death in addition to fractures, kidney stones, renal disease, depression, and cognitive impairment,” corresponding of the study Paul M. Bunch, MD, of the Department of Radiology at Wake Forest School of Medicine, and co-authors shared.
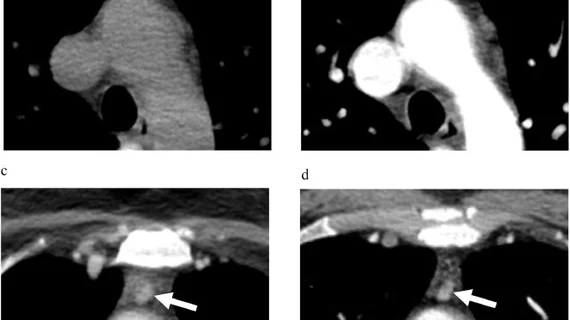
The researchers explained that due to the nature of PHPT diagnoses, radiologists do not routinely include the parathyroid gland in their search patterns. However, new developments in CT have opened doors for earlier identification of enlarged parathyroid glands based on estimated weight. Authors of the study hypothesized that habitually using these tools to assess parathyroid glands during routine contrast-enhanced CT (CECT) scans of the neck and chest could lead to earlier diagnosis and treatment of PHPT.
To test their theory, the researchers analyzed 38 patients undergoing parathyroidectomy who had completed CECT scans prior to biochemical screening. A single neuroradiologist examined the scans for gland enlargement and correlated findings with operative and pathology reports.
Through this they found that 76% of patients had enlarged parathyroid glands prior to biochemical screening. These findings predated diagnoses by an average of 30 months. For 90% of these patients, PHPT was pathologically confirmed and 46% developed at least 1 renal, bone or neurocognitive comorbidity.
“Enlarged parathyroid glands are frequently visible on routine CECTs acquired years prior to PHPT diagnosis. Screening for PHPT based on enlarged glands could potentially prevent associated complications in almost half of such patients,” the authors wrote, before cautioning that additional research is still warranted.
View the full study in Academic Radiology.
More on incidental findings:
Managing incidental radiologic findings: ACR-led initiative proposes several recommendations
Free-text radiology reports hold clues for managing incidental pancreatic lesions
Subspecialty radiologists disagree with non-specialists’ incidental nodule guidance in 38% of cases
Experts call for more structured reporting after study reveals wide variances in radiologist reads