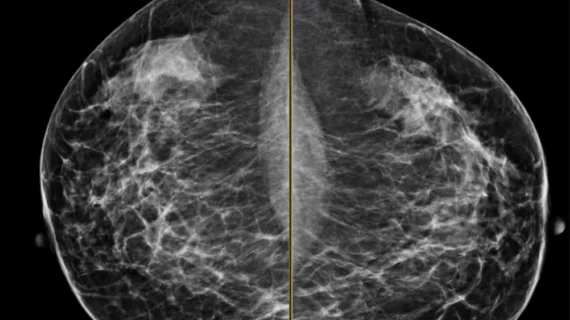
ACR, SBI launch screening mammo offense
A study published March 18 in Annals of Family Medicine that detailed long-term psychosocial harms of false-positive screening mammograms is compromised by methodological irregularities, underplays the harm of a breast cancer diagnosis and does not address existing strategies used to minimize anxiety, according to statements by the American College of Radiology (ACR), the Society of Breast Imaging (SBI) and breast imaging experts.
Methodology called into question on mammgrams leading to false-positives
The researchers expanded on prior studies and noted that patients experience varying levels of anxiety regarding test results and that these differences decline over time. However, there are too many methodological questions and irregularities in this analysis to accept the authors’ conclusion that anxiety is worse or more prolonged than previous studies concluded, according to the ACR and the SBI. For instance:
- Which (and how many) women with false-positive results (compared to those with normal results) had a family history of breast cancer? Those with a family history are more likely to have a positive test result. A positive test, and a family history, would be expected to elevate concern.
- Which (and how many) women with a false-positive exam were put into shorter-term surveillance (e.g., given more frequent mammograms)? They now have normal test results, but may not have been returned to the normal screening pool. Short-term surveillance is for women at higher risk. This would likely raise anxiety.
- Which (and how many) women with abnormal test results had a biopsy? This would likely increase anxiety compared to those who solely had a repeat mammogram or ultrasound. These women should be regarded as a third group since they affect overall scores of a group that initially had only a false-positive imaging exam.
- Which (and how many) women in the normal and abnormal groups had positive test results on their next round of screening? Was this cancer (cancer is more likely among those with a positive baseline test)?
The authors correctly cited that taking the survey under different conditions (women with normal results took the baseline survey at home, whereas women with abnormal results took it in the clinic) may have introduced bias. They guessed that bias among women with abnormal results would tilt toward less stress. One could certainly argue that the opposite was true, the statement continued.
“This study is missing critical details that make it difficult to broadly apply the authors’ results. Radiologists and primary care physicians are certainly aware that some patients will experience anxiety from any medical test. Radiologists are aware that it is important to minimize the number of patients recalled for further evaluation and biopsy,” added Barbara Monsees, MD, chair of the ACR breast imaging commission.
Striking a risk-benefit balance in the fight against false-positive mammograms
“False positive #mammogram? Existential crisis. False negative? #BreastCancer.” The early morning Tweet from Rich Duszak, MD, CEO of the Harvey L. Neiman Health Policy Institute, captured the emotional and medical consequences of screening outcomes.
Both the risks and benefits of screening mammography need to be considered, the breast imagers argued. “For women whose cancers are detected earlier because of mammography, the benefits are important and include a lower risk of dying of breast cancer. We need to help women get that benefit,” wrote Monsees.
One key to that benefit is communication. “Specific ways to decrease anxiety might be to reassure women when they are informed that they need to return for additional workup. They can be told by their primary care provider that most women recalled need only a few additional mammography views or an ultrasound, and that most of the time, they are then told that they are fine. Radiologists should make every attempt to make appointments readily available so that women don't have to wait long to get an appointment for their additional imaging. And at the time of repeat imaging, results should be given promptly, and personal reassurance can be provided,” wrote Monsees.
The ACR and the SBI also stressed ongoing work to reduce the number of false-positive exams.
“These findings do not call into question the value of mammography, but remind medical professionals that some women experience after effects of a false-positive exam,” the organizations concluded.